| |
| |
| |
| Presented By the Healthcare Distribution Alliance |
| |
| Axios Vitals |
| By Tina Reed · Feb 07, 2023 |
| Good morning, Vitals readers. Today's newsletter is 981 words or a 3½-minute read. 💻 Well, that didn't take long: Google is rolling out a test version of its AI bot to rival ChatGPT named ... "Bard." (Bard?) - "Whether it's helping doctors detect diseases earlier or enabling people to access information in their own language, AI helps people, businesses and communities unlock their potential," Sundar Pichai, CEO of Google and Alphabet said in his blog about the product on Monday.
|
| |
| |
| 1 big thing: Immunocompromised are left behind |
 Data: KFF; Chart: Thomas Oide/Axios The end of the COVID public health emergency is near, but that's small consolation to the estimated 7 million to 10 million immunocompromised Americans who are soldiering on with a dwindling number of tools to protect them, Axios' Sabrina Moreno and I write. The big picture: The immunocompromised — estimated to make up about 3% of Americans — have largely been an afterthought throughout the pandemic, patient advocacy groups say. - And with masking and social distancing increasingly in the rearview, there's a concern America is moving on without recognizing the needs of those who remain at high risk.
What they're saying: "People who are immunocompromised don't have that luxury," Lynn Albizo, vice president of public policy at the Immune Deficiency Foundation told Axios. Driving the news: Last month, the FDA pulled its emergency use authorization for the antibody treatment Evusheld, which helped bolster immunocompromised defenses, saying it worked on fewer than 10% of the circulating variants in the U.S. causing infection. - The loss of the authorization came on the heels of a study published in Cell in December, which found "all clinical monoclonal antibodies were rendered inactive against these variants." The FDA pulled its authorization for another monoclonal in late November.
- "The withdrawal of Evusheld is a disaster for our immunocompromised patients and illustrates the hard fight ahead against this virus," Arturo Casadevall, chairman of Johns Hopkins School of Public Health department of molecular microbiology and immunology, wrote on Twitter.
The bottom line: Clearly, COVID is a very different disease than three years ago with more widespread natural immunity, vaccines and treatments that are effective on broad swaths of the population, Leana Wen, an emergency physician and public health professor at George Washington University, said in a Washington Post opinion. - It's all the more reason that as we unwind COVID-era policies, the country should concentrate on efforts to find ways to protect the most medically vulnerable, she argued.
Read the rest. |
    |
| |
| |
| 2. Biden previews SOTU health asks |
 |
|
| President Joe Biden. Photo by Andrew Caballero-Reynolds/AFP via Getty Images |
| |
| President Biden's State of the Union address will include calls for insulin cost caps for privately insured patients and a renewed bid to close the Medicaid coverage gap in Republican-controlled states that haven't accepted the Affordable Care Act's Medicaid expansion, Axios' Adriel Bettelheim writes. The big picture: Neither proposal has much of a chance, but the speech gives Biden a chance to draw contrasts with Republicans and highlight policy successes in the Inflation Reduction Act, according to Larry Levitt, executive vice president of health policy at the Kaiser Family Foundation. Between the lines: Biden will revive ideas that were rejected during negotiations over the IRA. - The White House frames this as part of ongoing efforts to lower health care costs for working families and to "give more families the peace of mind of affordable prescriptions and health care."
Go deeper. |
    |
| |
| |
| 3. Judge gives Texas Medical Association a win |
| A federal judge ruled in favor of the Texas Medical Association on Monday in a challenge against HHS and its surprise billing rule. Driving the news: The U.S. District Court for the Eastern District of Texas ruled in favor of the medical association's motion for summary judgment in its lawsuit opposing certain components of the law. Catch up quick: This is one of four suits filed by the association challenging how the law, which seeks to prevent patients from getting stuck with surprise bills, requires insurers and out-of-network providers to work out billing disputes. The details: The TMA filed this lawsuit in September alleging the final rule favored insurers over providers in payment disputes. - In this case, the TMA challenged language in the final rule which required arbitrators to consider what's known as a qualifying payment amount, which the association alleges unfairly weights the process in insurers favor.
- HHS argued in December the final rule doesn't say arbiters must defer to the QPA, saying they're told to use "the offer that best represents the value of the item or service, regardless of whether that offer happens to be closest to the qualifying payment amount," Healthcare Dive reported.
- U.S. District Judge Jeremy Kernodle ordered provisions of the final surprise billing rule be tossed out.
|
    |
| |
| |
| A message from the Healthcare Distribution Alliance |
| Ensuring the availability of COVID-19 treatments in 2023 |
| |
 |
| |
| This year, more and more COVID-19 vaccines, PPE and therapeutics will likely shift to commercial sales. What this means: Healthcare distributors are ready to play an essential role in reliably delivering these vital, life-saving products to the public. Learn more. |
| |
| |
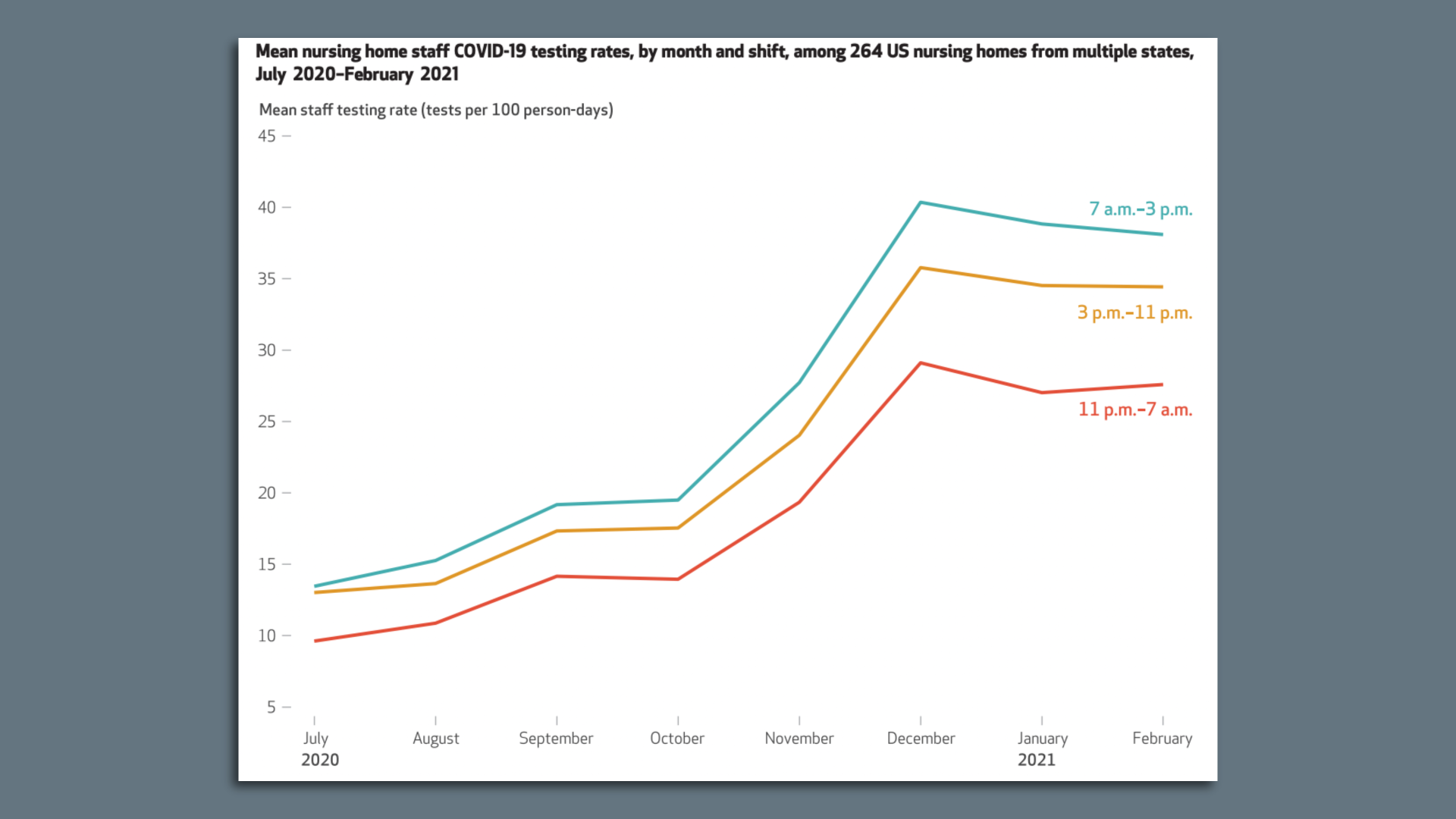
| 4. Data du jour: The difference a few hours can make |
 |
|
| Source: Health Affairs |
| |
| Night shift workers in nursing homes were tested for COVID-19 less often and were less likely to be vaccinated against the virus than those working at other times, a study in Health Affairs found. Why it matters: Nursing homes residents and workers were hit disproportionately with illness and death during the COVID pandemic and this study zeroes in on one place where their efforts were highly variable despite ongoing guidance from the CDC and CMS regarding who to test and when. Zoom in: The researchers, led by Brown University, looked at staff-level data, including time card data and logs of COVID-19 shots and testing, from a multi-state sample of 294 nursing homes between April 2020 and March 2021. - They found those on the shifts between 11pm and 7am had the lowest COVID-19 testing rates and lowest odds of COVID-19 vaccination.
- The testing trend held true across several months, even as testing became significantly more available in early fall 2020.
- "When staff testing and vaccination rates are lower on the evening and night shifts than on the day shift, that's an important weakness in the line of defense to be aware of and address," Elizabeth White, assistant professor of health services, policy and practice told Axios.
The bottom line: While this was a COVID-specific study the findings also suggest a broader need "to coordinate resources" for any shift-based workforce, White said. |
    |
| |
| |
| 5. Catch up quick |
 |
|
| Photo: Burak Kara/Getty Images |
| |
| 🏥 Hospitals were inundated with patients — and in some cases, seriously damaged themselves — as a result of a 7.8 magnitude earthquake that hit Turkey and Syria on Monday. (Los Angeles Times) 👉 What the end of the public health emergency means for Title 42. (Politico) 👀 The U.K.'s government-run health care service is in crisis. (Wall Street Journal) |
    |
| |
| |
| A message from the Healthcare Distribution Alliance |
| Making the pharmaceutical supply chain more resilient |
| |
 |
| |
| A more resilient supply chain requires enhanced collaboration between the public and private sector. What you need to know: Healthcare distributors have been working with supply chain and government partners to build on our collective strengths and identify ways to enhance resilience. Read more. |
| |
| Did someone forward this email? Subscribe here. Thanks for reading, and thanks to senior editor Adriel Bettelheim and senior copy editor Bryan McBournie for the edits. |
 | | Your personal policy analyst is here. | | |
No comments:
Post a Comment