| |
| |
| |
| |
| |
| Axios Vitals |
| By Tina Reed · Aug 18, 2022 |
| Good morning, Vitals readers. 💩 We'll start with 1 interesting thing: Curious about all this ado about wastewater and disease surveillance? The New York Times now has a "photographic journey" showing how it works. - Yes, they even have "the gross part."
With that, on to today's newsletter, which is 851 words or a 3-minute read. |
| |
| |
| 1 big thing: CDC's fix-it plan is good, but not enough |
 |
|
| Illustration: Megan Robinson/Axios |
| |
| Public health experts say the CDC's new plan to reform itself is generally a good plan — but without much bigger, more fundamental changes, the U.S. might continue to be caught flat-footed by new threats, Axios' Caitlin Owens writes. The big picture: Systemic failures at the CDC have sown public distrust in health experts over the past three years, but America's public health problem is much bigger than any one agency — and the politicization of the COVID pandemic only made things worse. Driving the news: The CDC yesterday vowed to change course after COVID thrust its shortcomings into the spotlight. - The agency's diagnosis of itself as too slow, too academic and too confusing to the public is spot-on, experts told Axios.
- "It is undeniably right that a system that is set up to deal with a relatively stable status quo is not equipped to handle rapid change. This recognizes that," Harvard epidemiologist Bill Hanage said.
State of play: The country's public health problems are piling up. - COVID-19 still kills around 400 people a day in the U.S., and around 100,000 new cases are still being reported each day.
- Meanwhile, experts are losing hope that monkeypox can be contained, at least in the short term, after the U.S. fumbled its initial response.
- A polio case was recently detected in New York, the first reported case since 2013. Wastewater samples indicate the virus may have been circulating since as early as April.
- Vaccine rates for other diseases plummeted during the pandemic and anti-vaccine sentiment is on the rise.
- On top of all that, the country's public health workforce is short-staffed and burned out.
The bottom line: How the CDC's reforms are implemented will be crucial, experts say, and there's plenty of work outside of the agency to be done. Go deeper. |
    |
| |
| |
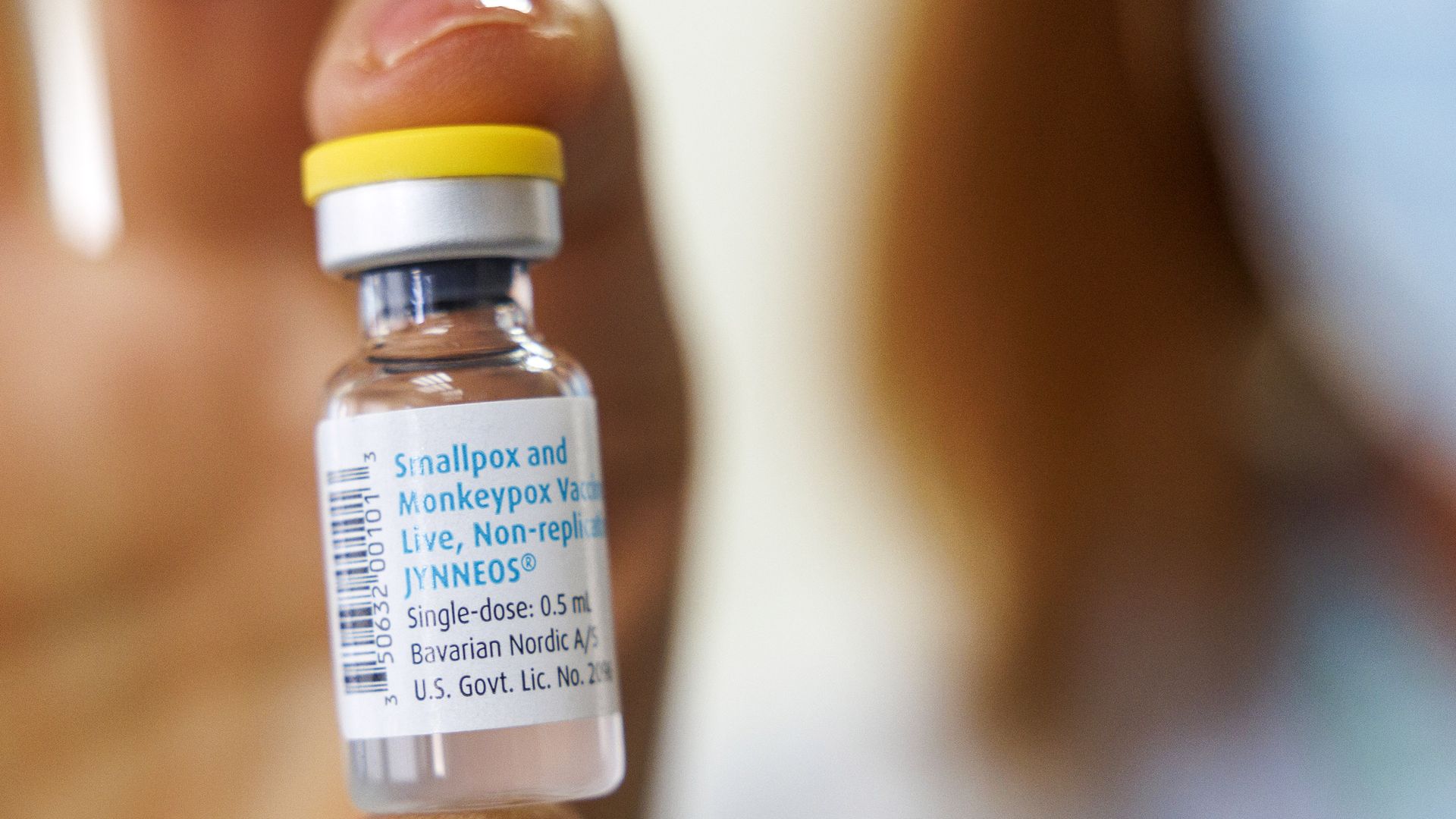
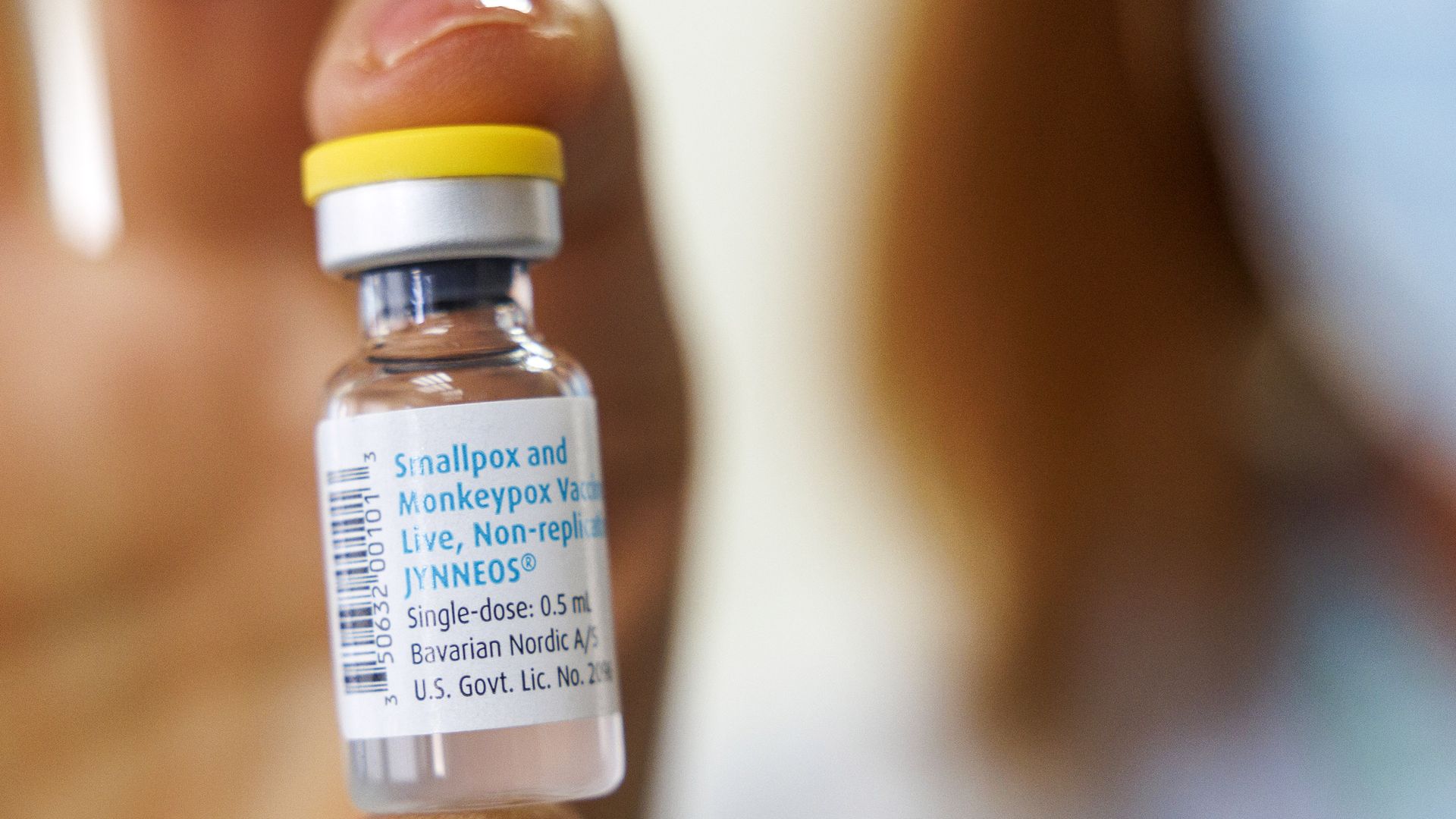
| 2. Scramble to make more monkeypox vaccine |
 |
|
| Photo: Kobi Wolf/Bloomberg via Getty Images |
| |
| Bavarian Nordic, the manufacturer of the world's only monkeypox vaccine, is unsure it'll be able to keep up with the demand for the shots, Bloomberg reports. Why it matters: The company, which produces the vaccine Jynneos, is searching for partners to help it quickly ramp up production, a move it previously said would be too cumbersome and expensive, per Bloomberg. - "Demand keeps rising and it's no longer certain that we can continue to meet the demand we're facing even with the upgrade of our existing manufacturing site in Denmark," Rolf Sass Sorensen, a vice president at Bavarian Nordic, told Bloomberg on Wednesday.
State of play: Infections jumped 20% over the last week, according to the World Health Organization. - There are now more than 35,000 confirmed cases total in 92 countries worldwide.
Zoom in: This week, the U.S. increased its contract with the company for Jynneos vaccines to $1 billion as HHS announced it would make 442,000 new doses available for states. - Bavarian Nordic has previously said it has the capacity to make 30 million to 40 million doses of Jynneos. However, some experts say they believe the company's true capacity is likely as low as 20 million, NPR reported.
|
    |
| |
| |
| 3. FDA approves $2.8M gene therapy |
| The FDA yesterday approved Zynteglo, a gene therapy from Bluebird Bio that treats patients with the blood disorder beta-thalassemia. Why it matters: The one-time treatment — which helps patients who depend on regular blood transfusions and face decreased life expectancy — comes at a record price of $2.8 million. - It's only the third gene therapy approved by the FDA.
Details: Bluebird estimates there are between 1,300 and 1,500 people with beta-thalassemia, also known as beti-cel. - The company plans to use an outcome-based agreement, saying it'll reimburse insurers up to 80% of the cost of the therapy for any patients who still need regular transfusions after their treatment.
What they're saying: The Institute for Clinical and Economic Review, a group that evaluates drug pricing and effectiveness, said in a statement the drug has high long-term value, even with a price tag over $2 million. The bottom line: Gene therapies offer a particular source of promise for treating rare diseases. But they've proved costly so far and the growing pipeline of such treatments could lead to staggering health care spending. |
    |
| |
| |
| A message from Axios |
| NEW: Subscribe to Axios Communicators |
| |
 |
| |
| Get the latest topics and trends impacting the way leaders, organizations and employers communicate. Why it matters: Axios Communicators will help inform your strategy and offer insight into the rapidly evolving world of sharing and receiving information. Subscribe for free |
| |
| |
| 4. Quote du jour |
 |
|
| Photo: Fabrice Coffrini/AFP via Getty Images |
| |
| "I haven't heard in the last few months any head of state talking about the Tigray situation anywhere in the developed world. Anywhere. Why? ... Maybe the reason is the color of the skin of the people in Tigray." — WHO Director-General Tedros Adhanom Ghebreyesus, speaking yesterday about the humanitarian crisis caused by the ongoing conflict in Ethiopia. |
    |
| |
| |
| 5. Pharmacies must pay $650M in opioids suit |
 |
|
| Photo: Paul Weaver/SOPA Images/LightRocket via Getty Images |
| |
| A federal judge yesterday ordered three of the country's largest pharmacy chains — CVS, Walgreens and Walmart — to pay $650 million to two Ohio counties, claiming the way they distributed opioids caused severe harm and created a public nuisance, Axios' Laura Martinez writes. Why it matters: It is the first ruling by a federal judge to put a price tag on pharmacies' role in the opioid crisis. What's next: CVS, Walmart and Walgreens disagreed with the court decision and said they will appeal. |
    |
| |
| |
| A message from Axios |
| NEW: Subscribe to Axios Communicators |
| |
 |
| |
| Get the latest topics and trends impacting the way leaders, organizations and employers communicate. Why it matters: Axios Communicators will help inform your strategy and offer insight into the rapidly evolving world of sharing and receiving information. Subscribe for free |
| |
 | | Why stop here? Let's go Pro. | | |






No comments:
Post a Comment