| |
| |
| |
| Presented By PhRMA |
| |
| Axios Vitals |
| By Tina Reed · Jul 06, 2022 |
| 🐫 Good morning, Vitals readers. Yep, we've made it to midweek already. Situational awareness: The Omicron subvariant BA.5 is now the dominant variant circulating around the U.S., accounting for nearly 54% of new cases, per CDC data. Today's newsletter is 951 words, a 3,5-minute read. |
| |
| |
| 1 big thing: A national bidding war for ARPA-H |
 |
|
| Illustration: Gabriella Turrisi/Axios |
| |
| An interstate bidding war has broken out for the chance to house the headquarters of a multibillion-dollar new science agency aimed at curing major diseases — before the agency's structure has even been finalized by Congress, Axios' Emma Hurt writes. Why it matters: The Advanced Research Project Agency for Health, or ARPA-H, is a pet project of President Biden's that would focus on breakthrough health care and technology innovations, looking for and finding ways to cure cancer, Alzheimer's disease, diabetes and more. Driving the news: States and cities including Georgia, Massachusetts, North Carolina, Cleveland, Texas and Philadelphia have made or plan to make pitches to the Department of Health and Human Services, many through bipartisan letters from their congressional leaders. State of play: While the agency's director will report to the secretary of Health and Human Services, the exact structure remains undecided. The Biden administration envisioned ARPA-H as being housed within the National Institutes of Health, in part for efficiency. But a bill the House passed in June would make it a stand-alone agency. The Senate has yet to take up the matter. - The agency is being modeled after the Pentagon's research arm, DARPA.
- Rep. Anna Eshoo (D-Calif.), who sponsored the House bill, sees the agency as "nimble, dynamic and independent," a view echoed by others in Congress who've questioned whether NIH's culture could support a more risk-taking entity.
The big picture: A spokesman for the department told Axios they "have made no commitments as to the physical location of ARPA-H. The decision on its location will ultimately be up to the inaugural director in consultation with the secretary." Yes, but: An inaugural director has yet to be named. Read the rest. |
    |
| |
| |
| 2. Prenatal screening risk in post-Roe landscape |
 |
|
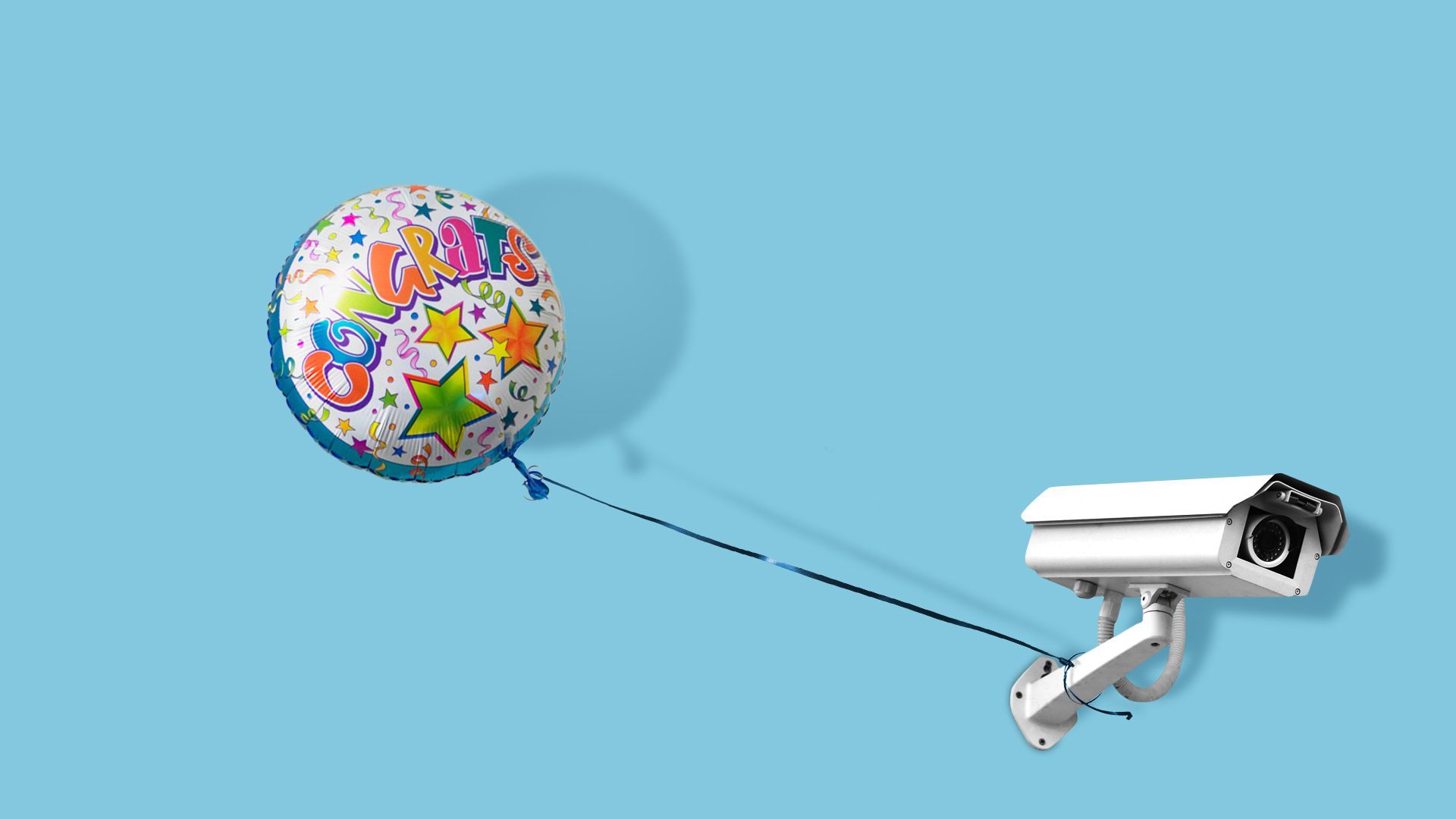
| Illustration: Natalie Peeples/Axios |
| |
| Pregnant people who get routine prenatal screening may be at risk of prosecution in states with strict new abortion bans, even if they plan to continue the pregnancy, Axios' Adriel Bettelheim writes about a commentary in Cell Reports Medicine. The big picture: It's another way the overturning of Roe v. Wade is subsuming other forms of reproductive health care. Driving the news: Some state prohibitions on abortion limit the right to end a pregnancy based on the information learned from ultrasounds and blood tests about the predicted sex of a fetus or genetic conditions like Down syndrome. - Deliberately vague legal language would prevent the return of results to any person willing to consider termination because any abortion after a positive result could be prosecuted, the authors from the Mayo Clinic and Case Western Reserve University write in a commentary out Tuesday.
- Prohibitions could also impact assisted fertility services like pre-implantation genetic screening used to detect embryos affected by inherited conditions like Tay-Sachs and Huntington's disease.
What they're saying: "Even families who do not want to terminate a pregnancy affected by a particular genetic trait may find themselves under increased surveillance and suspicion throughout the pregnancy and beyond," the authors write. |
    |
| |
| |
| 3. 1 in 5 Healthcare.gov claims denied: KFF |
 Reproduced from KFF; Chart: Axios Visuals Nearly one in five claims submitted for in-network services were denied by Healthcare.gov marketplace insurers in 2020, a Kaiser Family Foundation analysis found. Why it matters: The marketplaces, created under the Affordable Care Act, were aimed at improving access to insurance coverage — but in-network coverage is often being denied and customers rarely challenge those decisions. The details: Researchers analyzed CMS data on more than 230 million claims submitted to 144 insurers selling marketplace coverage in 2020, KFF said. - They found huge variations among plans, with some denial rates as high as 80% while others were as low as 1%.
- Insurers within the same state also often showed big differences.
Zoom in: The researchers said it's unclear why the in-network denial rates are so high, but many fall into a broad category of "all other reasons" which likely includes paperwork errors. Other reasons included lack of prior authorization (10%.) |
    |
| |
| |
| A message from PhRMA |
| Voters want Congress to address health insurance |
| |
 |
| |
| Many Americans reject so-called government "negotiation" once they learn it could sacrifice access, choice and innovation. The story: Respondents find health care coverage costs unreasonable and a top priority health care issue for policymakers to address today. Read more in the new survey. |
| |
| |
| 4. COVID still among top causes of death |
 Data: Shiels MS, Haque AT, Berrington de González A, Freedman ND. Leading Causes of Death in the US During the COVID-19 Pandemic, March 2020 to October 2021. JAMA Intern Med. Published online July 5, 2022. doi:10.1001/jamainternmed.2022.2476; Chart: Axios Visuals COVID-19 was the third leading cause of death in the U.S. in 2020 and 2021, accounting for one in eight lives lost, Adriel writes about a new review of death certificate data in JAMA Internal Medicine. Why it matters: The virus exacted a huge human toll even after vaccines became widely available and indirectly affected other causes of death like heart attacks and strokes, in part by discouraging some Americans from seeking care. - Our thought bubble: The true toll, in all likelihood, was significantly higher. Some COVID-19 deaths were misattributed to other causes. And the analysis didn't cover the Omicron wave of late 2021 and early 2022.
|
    |
| |
| |
| 5. 1 big number |
| One in seven Americans who use insulin hit "catastrophic spending" levels in 2017-2018, meaning they spent more than 40% of their post-subsistence family income on insulin alone, according to a new study in Health Affairs. Zoom in: Catastrophic spending was 61% less likely among Medicaid beneficiaries than among Medicare beneficiaries. - That suggests factors other than income, such as different types of insurance coverage, are at play, the authors said.
|
    |
| |
| |
| 6. Hospital readmission rates tied to nursing homes |
 |
|
| Illustration: Brendan Lynch/Axios |
| |
| Medicare patients less frequently needed to be readmitted after hospital stays in communities that had more nursing home beds and primary care physicians, Axios' Arielle Dreher writes about a new Health Affairs study. Why it matters: Hospitals can be penalized when patients cycle through their doors repeatedly under the federal Hospital Readmissions Reduction Program. - But that program does not account for the local continuum of care that hospitals rely on to take their discharged patients, the study authors write.
The bottom line: Understanding hospitals' discharge options in their markets could improve the CMS algorithm used in the Hospital Readmissions Reduction Program, according to the study. - It could "lead to lower readmission targets" for hospitals that operate in regions with more nursing homes and primary care providers, as well as lead to more generous allowances for hospitals with more home health agencies in their community.
|
    |
| |
| |
| A message from PhRMA |
| Insured Americans face barriers to care |
| |
 |
| |
| Nearly half of insured Americans who take prescription medicines encounter barriers that delay or limit their access to medicines. Learn more about the abusive insurance practices that can stand between patients and the care they need in PhRMA's new report. |
| |
 | It's called Smart Brevity®. Over 300 orgs use it — in a tool called Axios HQ — to drive productivity with clearer workplace communications. | | |








No comments:
Post a Comment