Plus, the DOJ goes after Medicare Advantage | Monday, August 02, 2021
| | | | | | | Presented By Partnership for America's Health Care Future | | | | Axios Vitals | | By Caitlin Owens ·Aug 02, 2021 | | Good morning. Tina is back from vacation and will be back in your inbox tomorrow morning. Thanks for letting me make a guest appearance! Today's word count is 893, or a 3-minute read. | | | | | | 1 big thing: The double-sided risk of bad vaccine communication |  | | | Illustration: Aïda Amer/Axios | | | | The public conversation around who's at risk as the Delta variant continues to spread in the U.S. has gone off the rails, and it's very possible that it will just get worse. What we're watching: Even as experts and officials try to put vaccinated Americans' risk in context, the world is still gathering data on the vaccines' effectiveness. - Reassuring the majority of vaccinated Americans they d0n't need to freak out could backfire if it causes those who are at risk to let down their guard.
Driving the news: Public health experts spent the weekend trying to reassure vaccinated Americans that they're not at a high risk of coronavirus infection, and certainly not of hospitalization or death. - But at the same time, researchers around the world are trying to determine how much the vaccines' effectiveness against severe disease wanes over time, and some countries are going ahead with booster shots for immunocompromised and elderly people.
Between the lines: Risk may look a lot different for vaccinated nursing home residents and older Americans, especially those who received their shots early on, than a vaccinated 20-something without any health conditions. - The number of nursing home cases is rising, and breakthrough cases are more problematic in nursing homes, tweeted Ashish Jha, dean of Brown's School of Public Health.
- "A breakthrough infection, which might be a nuisance for a healthy person, can be very serious for a frail person," he wrote.
The bottom line: The vaccines work extremely well, including against Delta, and the vaccinated are at much lower risk right now than those who aren't vaccinated. - But that doesn't mean no one who is vaccinated is at risk, and it also doesn't mean that anyone's risk can't change over time.
Go deeper. |     | | | | | | 2. Medicare Advantage further in the crosshairs | | The Department of Justice has joined whistleblower complaints that allege Kaiser Permanente knowingly made its Medicare Advantage patients look sicker than they were, as a way to obtain more money from the federal government. Why it matters: For years now the federal government has cracked down on fraudulent coding in Medicare Advantage. - But going after Kaiser Permanente, a company that many view as the gold standard for Medicare Advantage, indicates the problem may touch almost every corner of the industry, Axios' Bob Herman reports.
What they're saying: Kaiser knew many of its patients had inordinately high "risk scores," which help determine how much the federal government pays them, according to one of the unsealed lawsuits. But the company didn't fix the mistakes. - The other side: "We are confident that Kaiser Permanente is compliant with Medicare Advantage program requirements, and we intend to strongly defend against the lawsuits alleging otherwise," the company said in a statement.
The big picture: These allegations, which come against a consistent "five-out-five-star" plan, reinforce longtime expert warnings that Medicare Advantage insurers are bilking money by "upcoding" people's diseases. - For some insurers, risk scores were 20% above what they would normally be for similar patients who are enrolled in traditional Medicare "due to coding practices," the Medicare Advisory Payment Commission wrote in 2020.
The bottom line: Health insurers have railed against audits of their Medicare offerings, but increased DOJ involvement makes it appear there is continued gaming of this program. |     | | | | | | 3. LGBTQ patients' bad provider experiences |  Adapted from a KFF report; Chart: Connor Rothschild/Axios Over a third of LGBTQ Americans say they've had a negative experience with a health care provider over the past two years, according to KFF survey research. Why it matters: These findings, especially when coupled with the pandemic, should be a wake-up call about another big disparity in how the health care system treats different patients, KFF's Drew Altman writes in today's column. What they're saying: LGBTQ patients' negative experiences included providers not believing them, suggesting they were to blame for their health problems, making assumptions without asking, and outright dismissing their concerns. - Just 22% of non-LGBTQ patients reported similar experiences.
- The pandemic has also taken a disproportionate toll.
- LGBTQ workers were more likely to have had to quit their job because of the pandemic, and most of those who reported having problems paying medical bills in the past 12 months said it was at least in part because of the pandemic.
Between the lines: LGBTQ people are more likely to discuss mental health and non-medical issues such as housing or transportation with their doctors. The bottom line: There is an obvious need for more research and data to sort out what is behind these warning signals. - But it's clear that LGBTQ patients — who are disproportionately likely to have low incomes and chronic conditions — need a more responsive health care system.
Go deeper. |     | | | | | | A message from Partnership for America's Health Care Future | | Let's build on what's working, not threaten access to care | | |  | | | | As some politicians explore creating a new government-controlled health insurance system, research finds the public option could force hospitals to reduce critical services – disproportionately harming underserved communities. See the findings. | | | | | | 4. Quitting smoking after lung cancer diagnoses |  Data: Annals of Internal Medicine; Chart: Axios Visuals Patients who quit smoking after a lung cancer diagnosis lived an average of nearly 22 months longer than those who continued smoking, according to a study published last week in the Annals of Internal Medicine. Details: Researchers looked at patients who had been diagnosed with non-small cell lung cancer, which accounts for more than 85% of cancers and is associated with cigarette smoking, over a seven-year period of follow-up. They found patients who continued smoking lived, on average, less than five years beyond their diagnosis, Axios' Tina Reed writes. - Those who quit lived an average of 6.6 years.
A higher five-year overall survival rate and progression-free survival were also seen among patients who quit compared to those who kept smoking. - They found similar effects among mild-to-moderate and heavy smokers and those with earlier and later cancer states.
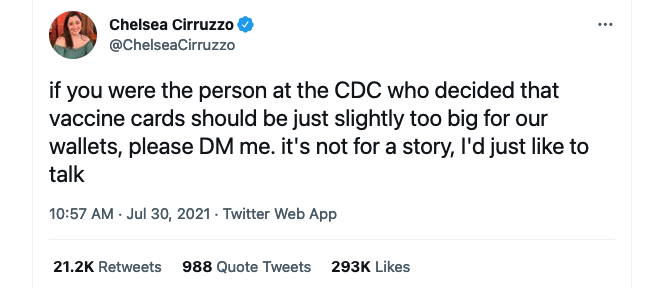
|     | | | | | | 5. Tweet du jour | Screenshot: @ChelseaCirruzzo (Twitter) |     | | | | | | A message from Partnership for America's Health Care Future | | Let's build on what's working, not threaten access to care | | |  | | | | Americans need lawmakers to build on and improve what's working in health care, not start over by creating a new government-controlled health insurance system like the public option that could threaten access to care for racial and ethnic minorities and rural Americans. Learn more. | | |  | | It'll help you deliver employee communications more effectively. | | | | | | Axios thanks our partners for supporting our newsletters. If you're interested in advertising, learn more here.
Sponsorship has no influence on editorial content. Axios, 3100 Clarendon Blvd, Suite 1300, Arlington VA 22201 | | | You received this email because you signed up for newsletters from Axios.
Change your preferences or unsubscribe here. | | | Was this email forwarded to you?
Sign up now to get Axios in your inbox. | | | | Follow Axios on social media:    | | | | | |








No comments:
Post a Comment