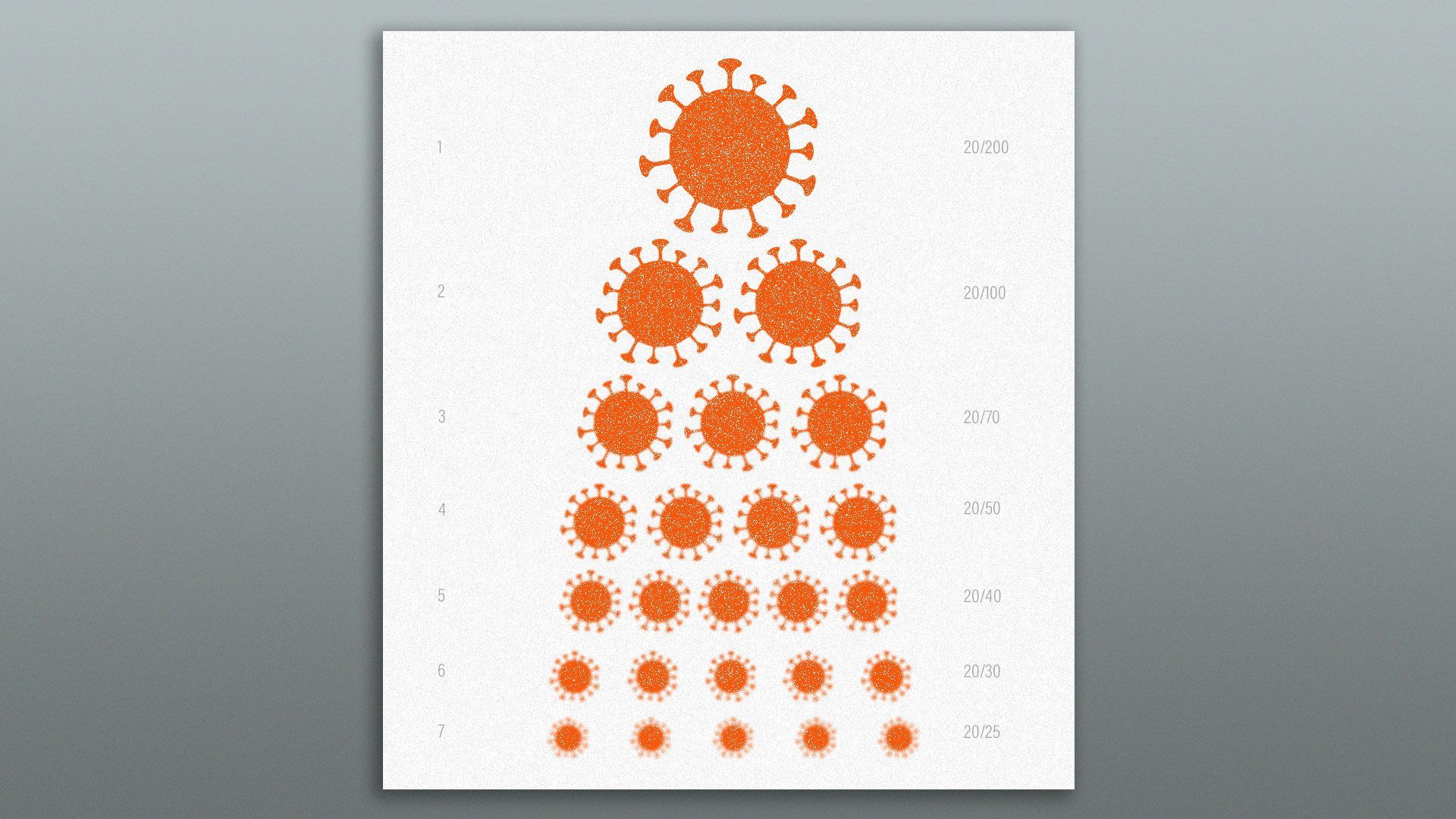
| | | | | | | Presented By PhRMA | | | | Vitals | | By Caitlin Owens ·Feb 01, 2021 | | Good morning. Today's word count is 1,052, or a 4-minute read. | | | | | | 1 big thing: Chilling trend: A longer, deadlier pandemic |  | | | Illustration: Eniola Odetunde/Axios | | | | Mutated versions of the coronavirus threaten to prolong the pandemic, perhaps for years — killing more people and deepening the global economic crisis in the process, Axios' Sam Baker writes. The big picture: The U.S. and the world are in a race to control the virus before these variants can gain a bigger foothold. But many experts say they already expect things to get worse before they get better. And that also means an end to the pandemic may be getting further away. Where it stands: "There are essentially two separate COVID-19 epidemics," Dutch officials said recently, referring to the original strain of COVID-19 and the burgeoning threat from mutated versions of the virus. - There's light at the end of the tunnel for the first epidemic. Although the virus is still spreading uncontrolled across the U.S. and much of the world, cases and hospitalizations are down from their peak, and vaccinations are steadily increasing.
- But the next iteration, fueled by variants of the virus, is already taking hold.
What's next: A British variant of the coronavirus will likely become the dominant strain within the U.S. pretty soon, experts say. It's significantly more contagious than the virus we've been dealing with so far, and some researchers believe it may also be about 30% more deadly. Vaccines work against the British variant, and they will help control its spread, just as they'll help control the pandemic overall. But vaccinations can only ramp up so quickly. - Vaccine makers can rework their recipes and come up with booster shots to help address more resistant strains, but that will take time.
How it works: All of these problems stem from the same underlying problem — the unchecked spread of the virus. Go deeper. |     | | | | | | 2. Essential workers bumped back in vaccine line | | When states decided to open vaccine eligibility more broadly to seniors, it bumped essential workers further down the vaccine line or forced them to compete with a new flood of people for shots, the Washington Post reports. Why it matters: Essential workers, who are disproportionately people of color, are at higher risk of infection than people who can more easily social distance. - Many frontline workers will now wait longer for protection from the virus.
The other side: Older people are generally at highest risk of severe disease or death from the virus. And opening up eligibility was intended to speed up the pace of inoculations — a crucial endeavor, as new virus variants begin to circulate in the U.S. Between the lines: The tradeoffs surrounding whether to vaccinate older Americans or essential workers first is yet another example of the tension between speed and equity. - "If the obsession is over the number of people vaccinated ... we could end up vaccinating more people, while leaving those people at greatest risk exposed to ongoing rates of infection," Richard Besser, president of the Robert Wood Johnson Foundation, told the Post.
- An advisory panel to the Centers for Disease Control and Prevention had initially recommended vaccinating people 75 and older and frontline essential workers in the second vaccine priority group, following health care workers and nursing home residents.
Go deeper: Teachers want the vaccine, but they'll have to wait |     | | | | | | 3. Life insurers screen for COVID-19 | 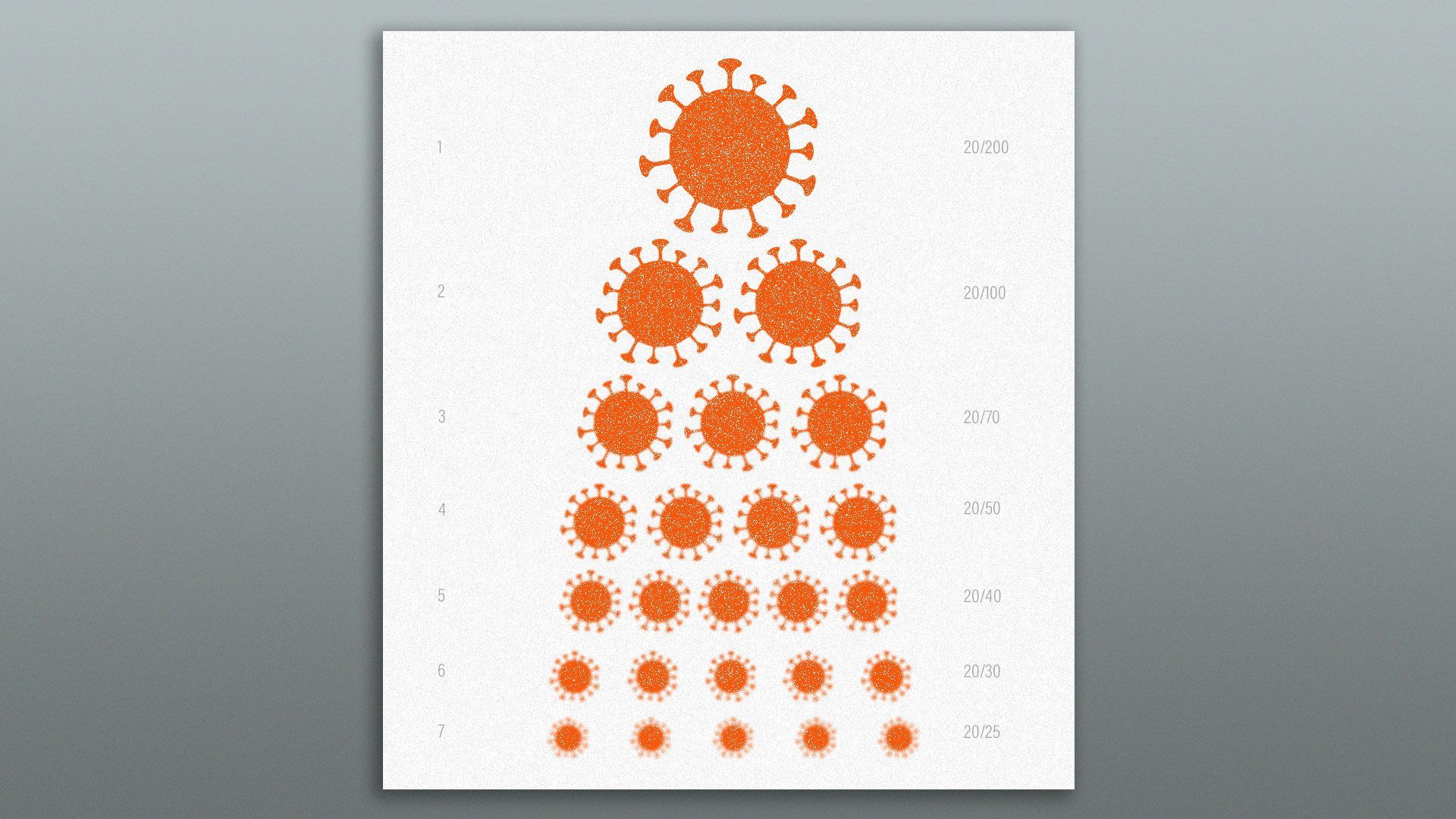 | | | Illustration: Eniola Odetunde/Axios | | | | Because of the pandemic, more people than ever are seeking out life insurance — just as insurers seek ways to identify people who have had COVID-19, and in some cases deny them coverage, Axios' Jennifer Kingson writes. Why it matters: If the coronavirus makes it harder for people to get life insurance — or to collect on existing policies — it could diminish access to an essential financial safety net. Driving the news: Alarmed at clampdowns by underwriters in Europe, the Consumer Federation of America (CFA) just sent a letter to the National Association of Insurance Commissioners urging that U.S. insurance firms establish clear and transparent rules on life insurance eligibility and COVID-19. - In Europe, some insurers impose 30-day waiting periods on applicants who are former COVID patients and limit coverage by age, the CFA letter said, citing a Reuters article.
What they want: The group says state insurance regulators "must issue a rule to protect consumers from arbitrary insurance practices." Where it stands: U.S. insurers are gingerly tweaking their underwriting rules. - In June, Bloomberg Law reports, insurers started filing requests with the Delaware Department of Insurance "to change their application forms to specifically ask applicants if they'd had COVID-19."
The bottom line: "Some reasonable precautions by life insurers are understandable, but to burden COVID patients and their families a second time is unjust and unfair," the CFA said. Go deeper. |     | | | | | | A message from PhRMA | | We are committed to being a part of the solution | | |  | | | | America's biopharmaceutical companies are committed to ending the pandemic by: - Continuing to develop treatments and vaccines to combat COVID-19,
- Working closely with governments, insurers and others to make sure vaccines and treatments are accessible and affordable.
| | | | | | 4. Trump admin vs. states on vaccine money | | Top Trump health officials urged Congress last fall not to give states any additional money for the coronavirus vaccine rollout, as state officials warned they didn't have the funding they needed, STAT scoops. Why it matters: The vaccine rollout was ultimately sluggish, and the number of vaccines administered in the first few weeks fell way short of federal projections — partially because states faced a lack of resources. - "Even after the Trump administration spent billions helping drug makers develop COVID-19 vaccines, it not only dismissed states' concerns about the help they would need to roll them out, but actively undermined their efforts to press Congress to get the funding they needed," STAT's Nicholas Florko writes.
What they're saying: Paul Mango, the former deputy chief of staff for policy at the Department of Health and Human Services, argued that states hadn't demonstrated they needed more funding, because they hadn't spent $200 million that the CDC sent to states in September. - In October, states asked Congress for $8.4 billion in funding.
Congress eventually passed a relief package that included $4.5 billion for state governments, but that money only began to flow to states in January. |     | | | | | | 5. The latest in the U.S. |  | | | Illustration: Aïda Amer/Axios | | | | Some of the richest countries in the world — the ones that had been considered the best prepared to handle a pandemic — turned out to be the ones that suffered the highest death rates, Axios' Felix Salmon reports. The effectiveness of the COVID-19 vaccines against disease and death has been remarkable, but too much emphasis on the unknowns about transmission could discourage people from getting vaccinated, Axios' Bryan Walsh writes. Maryland Gov. Larry Hogan announced Saturday that the potentially more transmissible coronavirus variant first discovered in South Africa has been identified in the state. The Centers for Disease Control and Prevention issued a public health order late Friday requiring face coverings on airplanes, trains and other public transportation to contain the spread of the coronavirus. The U.S. government spent almost $90 billion on Supplemental Nutrition Assistance Program benefits in fiscal year 2020, compared to the $60 billion price tag the year prior, according to data from the Agriculture Department released last week. High-end liquor gained its sharpest increase in sales in at least 40 years after the coronavirus pandemic brought lockdowns across the U.S., the Wall Street Journal reports. The Canadian government on Friday imposed fresh restrictions on international travel, banning flights to and from Mexico and Caribbean countries starting Sunday through at least April 30. New Zealand has avoided locking down for a second time over COVID-19 community cases because of a swift, science-led response, Axios' Rebecca Falconer reports. |     | | | | | | A message from PhRMA | | We are committed to being a part of the solution | | |  | | | | As we usher in a new Congress and new administration, we can all agree that people need quality, affordable health coverage that works when they need it. - We are focused on solutions that help patients better afford their medicines and protect access to innovation today and in the future.
| | | | | | Axios thanks our partners for supporting our newsletters.
Sponsorship has no influence on editorial content. Axios, 3100 Clarendon Blvd, Suite 1300, Arlington VA 22201 | | | You received this email because you signed up for newsletters from Axios.
Change your preferences or unsubscribe here. | | | Was this email forwarded to you?
Sign up now to get Axios in your inbox. | | | | Follow Axios on social media:    | | | | | |






No comments:
Post a Comment