| | | | | | | Presented By HCA Healthcare | | | | Axios Science | | By Alison Snyder ·Feb 03, 2022 | | Thanks for reading Axios Science. This week's newsletter is 1,632 words, about a 6-minute read. | | | | | | 1 big thing: "Next frontier" for pioneering cancer therapies |  | | | Illustration: Rebecca Zisser / Axios | | | | Cancer treatments that modify a patient's immune cells to attack cancer cells are being re-engineered to try to treat more cancers in more people. Why it matters: CAR-T immunotherapies have been successful in treating certain types of blood cancers in some people. But they struggle against solid tumors, which make up about 90% of cancers in adults. - "Solid tumors are the next frontier," says J. Joseph Melenhorst, an immunologist at the University of Pennsylvania who develops CAR-T therapies.
How it works: CAR-T cells are made by collecting a patient's T cells — one actor in the immune system — and reprogramming a receptor on the T cell surface to bind an antigen found on the surface of cancer cells. - Those reprogrammed cells are then put back into the patient, where they can attack the cancer cell.
- CAR-T therapies are approved by the FDA to treat some blood cancers and multiple myeloma.
- They've been successful in treating those cancers in some people, even those with advanced disease, but not all, and they are expensive and can have side effects, including releasing cytokines in the blood and affecting the nervous system.
The challenges: Solid tumors — including breast, prostate or lung cancers — are "almost impenetrable" for immune cells, Melenhorst says. - The T cells used in therapies need to enter the tumor's microenvironment — a hostile arrangement of blood vessels, proteins, and immune and other cells that surround a tumor, interact with it and influence its fate — to access the cancer cells.
- Another challenge: Solid tumor cancers can spread in the body and be difficult for T cells to find.
- And T cells can also become exhausted if they are exposed to the antigen they are targeting for prolonged times.
Both solid tumor and blood cancers can reemerge if cancer cells stop making the antigens on their surface that CAR-T cells target, allowing the cancer cells to evade the attacking immune cells. What's new: Scientists are experimenting with designing new CAR-T cells and therapies to find, attack and continuously surveil solid tumor cancers. - T cells are being engineered to target multiple antigens on a cancer cell in an effort to make it more difficult for cancer cells to escape and for cancers to return.
- But most of the antigen targets on solid tumors are also on types of healthy cells people can't live without, which poses safety concerns for patients.
A key aim for new CAR-T therapies is to be able to tailor their specificity. - "How to find an antigen that you can both safely target and use to effectively eliminate the tumor is a very challenging question," says Yvonne Chen, a scientist at UCLA who designs CAR-T cells.
- She and other researchers are exploring designing T cells that target cancer cells using an approach similar to logic gates in computing.
- CAR-T cells can be engineered to only attack a cell if it has one antigen but not another, making it more specific. But if it is too specific, cells of some types of cancer can slip by, prompting researchers to try to also program T cells to attack a cell that has one antigen or another one.
The bottom line: "Immunotherapy has promise for solid tumors, but there is a need for a lot more research to make solid cancers respond like blood cancers do," Carl June, an immunologist and oncologist at the University of Pennsylvania who led the early development of CAR-T therapy, said at a press conference this week. Read the full story. |     | | | | | | 2. A CAR-T "cure" |  | | | A lab technician works on a research process to find new CAR-T cells. Photo: Thomas Coex/AFP via Getty Images | | | | A decade after receiving an early CAR-T treatment, two patients who had a form of blood cancer show no signs of the disease, researchers reported this week. Why it matters: The patients' remissions hint at how long the effects of CAR-T therapy — a promising but currently very costly treatment— may persist in some people. - "We can now conclude CAR-T cells can cure patients with leukemia based on these results," June, an author of the paper published Wednesday in Nature, said in a press briefing earlier this week.
- "We need many more patients to be followed, but at least in these two patients there is no more leukemia."
What they found: Three patients with chronic lymphocytic leukemia — a slow progressing cancer that starts in the bone marrow and goes to the blood — received a CAR-T therapy in 2010 at the University of Pennsylvania as part of a clinical trial assessing the safety and effectiveness of the treatment. - Two patients went into complete remission that year.
- The researchers analyzed the patients' CAR-T cells over time, and found that 10 years later the cells continued to be active and surveilling for cancer cells — and no leukemia cells were detected, June said.
- The cells also evolved in the patients like normal T cells do: They went from active killer T cells to another type of immune cells called helper T cells that are bystanders but still able to kill cancer cells.
Keep in mind: The therapy doesn't work for all patients or all types of cancers. - The new study provides details about how the CAR-T cells work and researchers say it could help improve the therapy so that it is effective in more people.
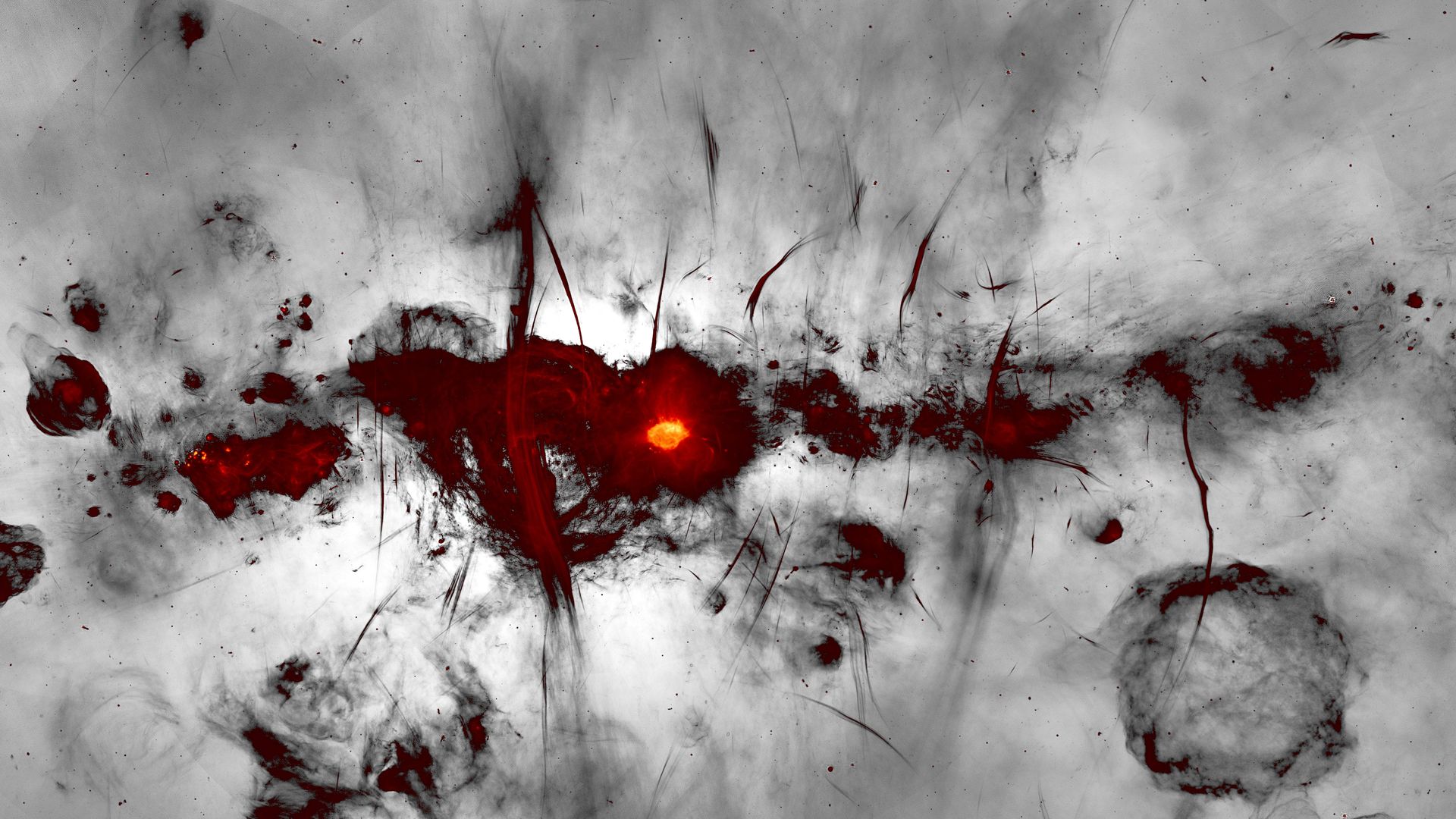
Go deeper. |     | | | | | | 3. Catch up quick on COVID |  Data: N.Y. Times; Cartogram: Kavya Beheraj/Axios "Omicron is finally on its way out, but it's leaving behind a death toll that is still rising," per Axios' Sam Baker and Kavya Beheraj. Moderna's COVID vaccine received FDA approval, Novavax filed a request to the FDA for emergency use authorization of its vaccine, and Pfizer asked the agency to green light the use of its vaccine in children under age 5. People infected with the original SARS-CoV-2 strain become infectious after two days — sooner than researchers thought, Clive Cookson and Oliver Telling report in the FT. The results are from the first COVID human challenge trial in which people are deliberately exposed to the virus. |     | | | | | | A message from HCA Healthcare | | HCA Healthcare strengthens partnership with March of Dimes | | |  | | | | Throughout 2021 and 2022, HCA Healthcare will contribute up to $1.7 million to March of Dimes. By working together, the two organizations are uniquely positioned to continue to improve maternal and postpartum care. Learn more about HCA Healthcare's commitment to showing up. | | | | | | 4. A "Category 6" hurricane simulator |  | | | Illustration: Annelise Capossela/Axios | | | | A trend toward rapidly intensifying, powerful huricanes in recent years is spurring experts to examine more closely how to prepare communities to better withstand such violent weather, Axios' Andrew Freedman reports. Driving the news: The U.S. National Science Foundation (NSF) recently awarded about $13 million over four years to Florida International University's (FIU) Extreme Events Institute to support the design of what is essentially a "Category 6" storm simulator. - The grant will allow FIU to create a testing facility capable of producing winds of up to 200 mph, complete with a water basin to simulate storm surge and wave activity.
Currently, the Saffir-Simpson Hurricane Wind Scale goes from Category 1 through 5, maxing out when a storm's top sustained winds go above 155 mph. - Yet many storms have intensified so significantly that they might as well be called Category 6 storms, though the broad meteorological community has not rallied around a push to add another number.
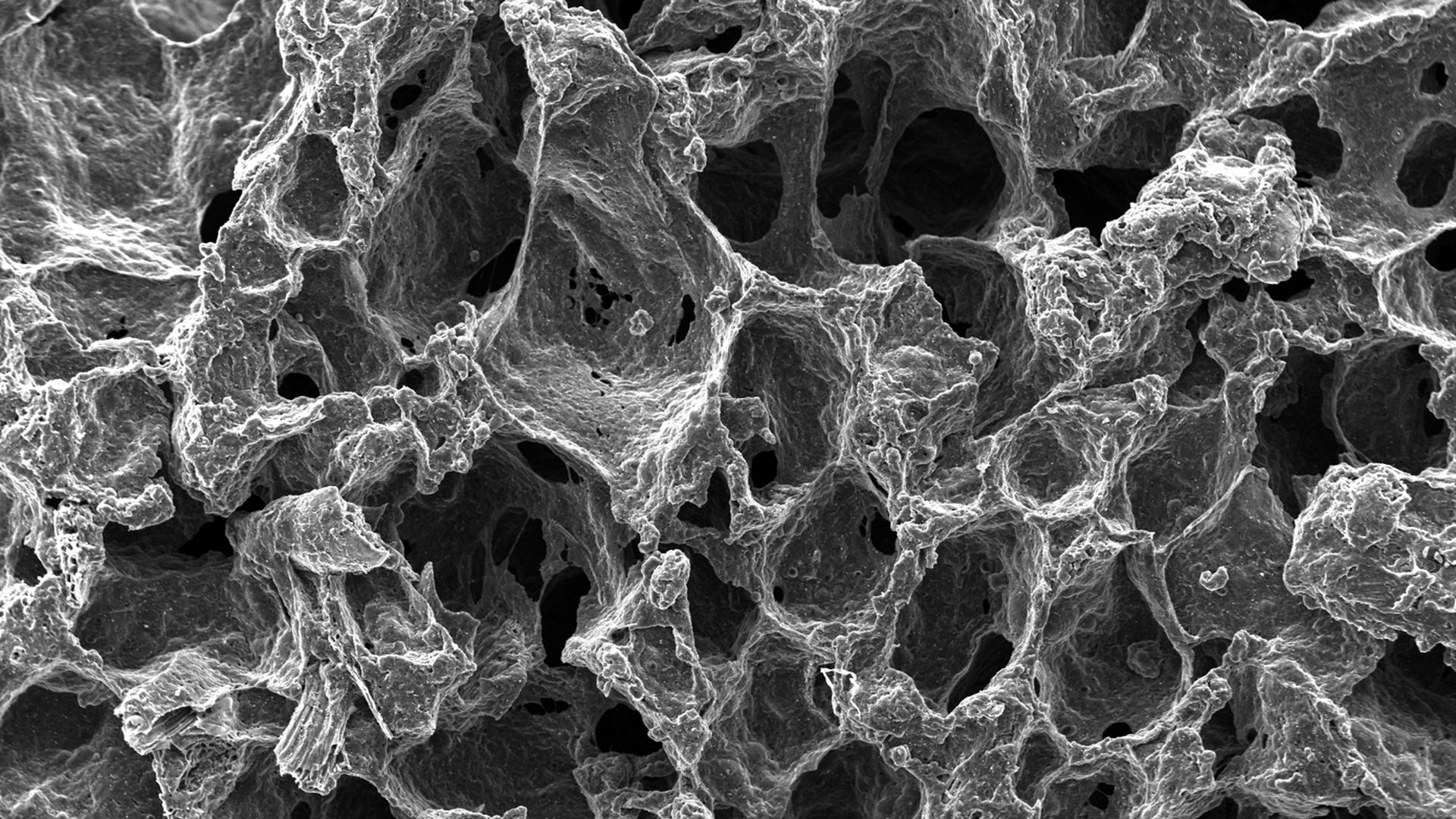
Details: The new facility at FIU, which will be more heavily outfitted than an ordinary wind tunnel, will be built with the participation of other colleges, including Colorado State University and the Georgia Institute of Technology, along with a private company, AeroLab. Read more. |     | | | | | | 5. Worthy of your time | 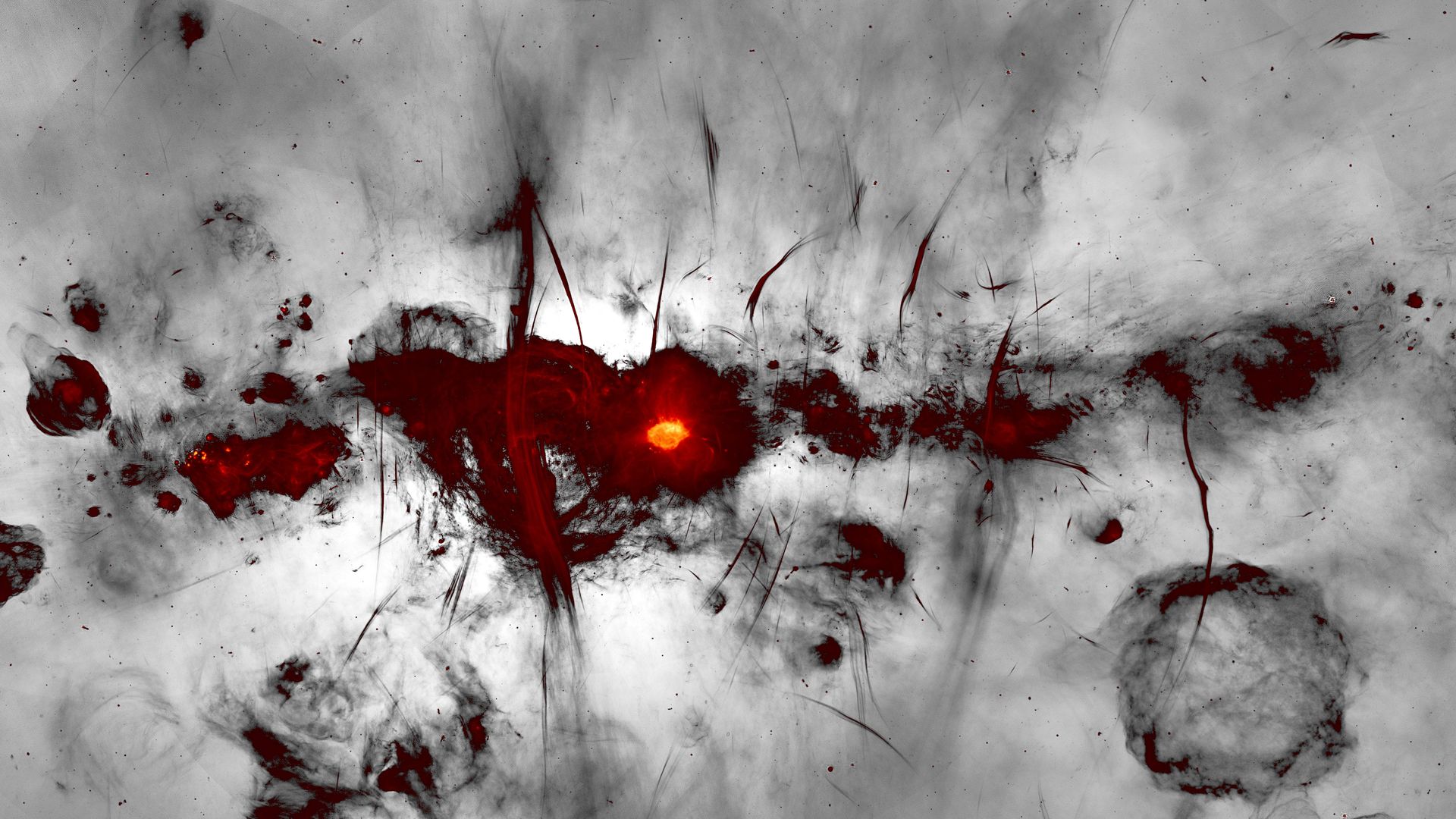 | | | A new radio image of the center of the Milky Way galaxy. Credit: I. Heywood/SARAO | | | | An electrifying view of the heart of the Milky Way (Dennis Overbye — NYT) The race is on to save the Great Salt Lake (Lindsay Whitehurst — AP) Wildfires' unequal impacts on pregnant women (Sarah Sax — High Country News) Plants in the U.K. now flowering a month earlier (Helen Briggs — BBC) |     | | | | | | 6. Something wondrous | 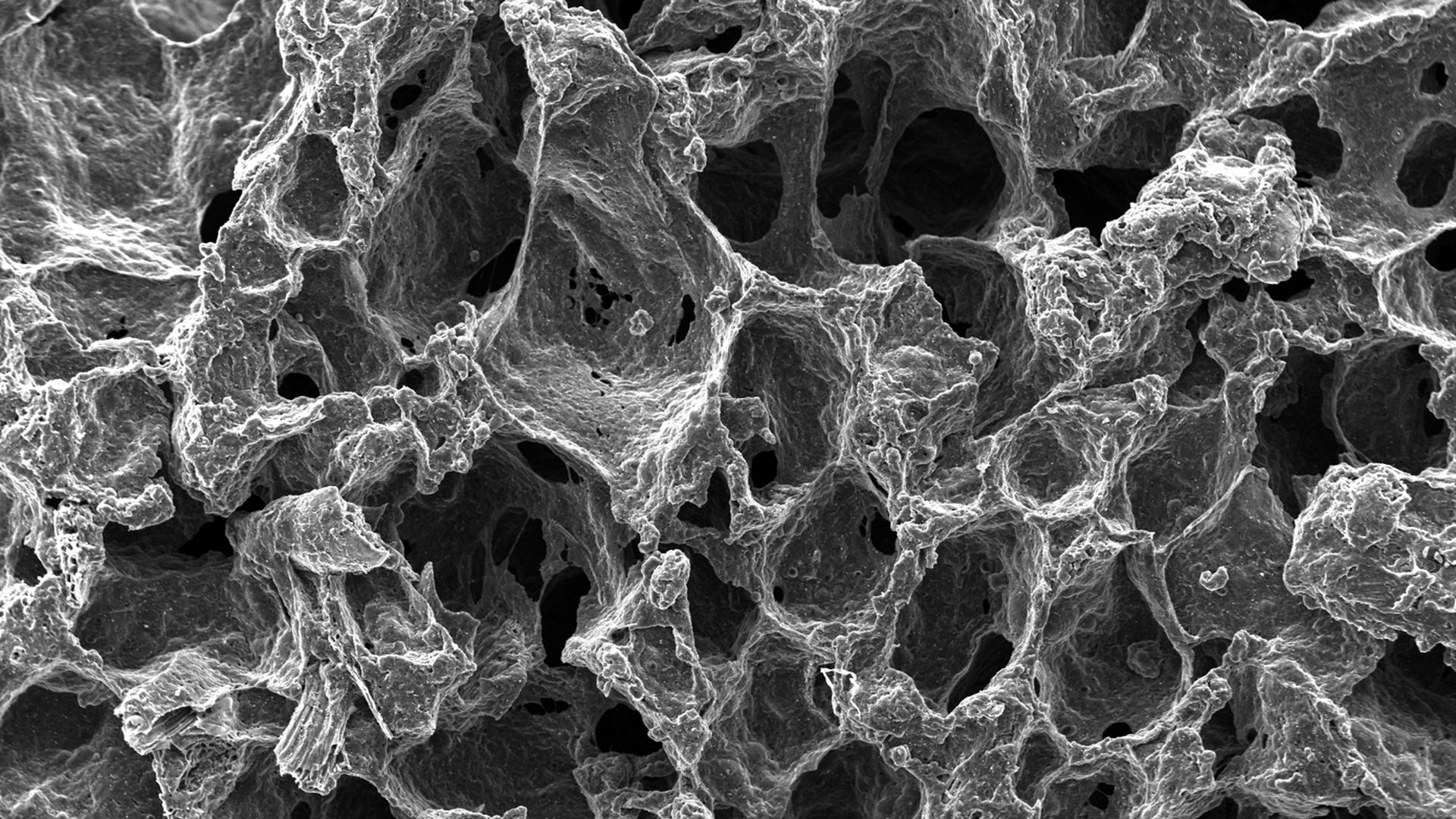 | | | Scanning electron microscope images of carbonized freestanding bread electrodes. Image: Adam Wood (Saint Vincent College) and Philip LeDuc (Carnegie Mellon University) | | | | Burnt bread could be used to remove salt from water, according to a new study. Why it matters: Desalination is one tool for addressing water scarcity in a world that is expected to become even more water-stressed. But the energy-intensive technology is expensive, and researchers are looking for new ways to take salt out of water. The idea of using bread to desalinate water sparked for Adam Wood, now an assistant professor of engineering at Saint Vincent College, as he watched an extra hamburger bun char in the center of a fire pit in his backyard. - Wood had been studying whether the roots of mangrove plants that turn saltwater into fresh water could be used as electrodes for capacitive deionization, a desalination technology.
- But mangrove roots have drawbacks — for one, they don't grow uniformly— so he started to look for other porous organic materials that could be used in their intact form.
- Typically electrodes — one of the most expensive components in the process — are made by pyrolyzing wood or other materials to make them conductive, then grinding them up, mixing them with other materials and packing them together.
When Wood saw the burning bun, he says, "it was turning into a carbon electrode right before my eyes." How it works: Capacitive desalination uses electrodes and a low voltage power supply, and requires a porous material that water can easily pass through. - Under more controlled lab conditions, Wood found bread could be used to create electrodes. It maintains its structure after about an hour of slow heating in the lab, he and Philip LeDuc, a professor of mechanical engineering at Carnegie Mellon University, reported in RSC Advances.
- They also experimented with carbonizing the bread in the field with different fire structures and wood that could be available in places where there are limited financial resources.
- When they hooked those field-baked bread electrodes up to an inexpensive solar panel, they found it could lower the salt concentration in brackish water by almost 60%, producing good drinking water by World Health Organization standards in about two hours.
- It's "performance in every aspect is better than mangrove roots — and on par with state of the art electrodes," Wood says.
But, but, but... Whether the bread-based desalination approach could be used on a large scale is unclear. Read more. |     | | | | | | A message from HCA Healthcare | | How HCA Healthcare shows up during times of crisis | | |  | | | | Whether facing a natural disaster or pandemic, HCA Healthcare's Enterprise Emergency Operations Center is ready to help. It works with experts to prepare and provide necessary resources like generators, water and housing to ensure the safety of their colleagues and uninterrupted patient care. | | | | Thanks to Amy Stern for copy editing this edition. |  | Bring the strength of Smart Brevity® to your team — more effective communications, powered by Axios HQ. | | | | | | Axios thanks our partners for supporting our newsletters. If you're interested in advertising, learn more here.
Sponsorship has no influence on editorial content. Axios, 3100 Clarendon Blvd, Suite 1300, Arlington VA 22201 | | | You received this email because you signed up for newsletters from Axios.
Change your preferences or unsubscribe here. | | | Was this email forwarded to you?
Sign up now to get Axios in your inbox. | | | | Follow Axios on social media:    | | | | | |







No comments:
Post a Comment