| |
| |
| |
| Presented By the Coalition Against Surprise Medical Billing |
| |
| Axios Vitals |
| By Tina Reed ·Aug 19, 2021 |
| Good morning, Vitals readers. Today's newsletter is 1,071 words, or a 4-minute read. - Join Axios justice and race reporter Russ Contreras and politics reporter Stef Kight today at 12:30pm ET for an Axios Latino event on adversity in health care and vaccinations.
- Guests include Rep. Veronica Escobar (D-Texas) and Juan J. Rivera, a practicing cardiologist and chief medical correspondent for Univision. Register here.
|
| |
| |
| 1 big thing: What the new vaccine data does and doesn't tell us |
 |
|
| Illustration: Shoshana Gordon/Axios |
| |
| The new coronavirus vaccine data released yesterday by the CDC confirms what other recent research has been saying: The coronavirus vaccines' effectiveness against infection has decreased over time, Axios' Caitlin Owens writes. Between the lines: There's little to no data that the vaccines' effectiveness against hospitalization will eventually follow suit. Driving the news: The CDC released three new studies focusing on the vaccines' effectiveness, particularly in light of the Delta variant. - One looked at Pfizer and Moderna's effectiveness against infections among nursing home residents over time, and found that it dropped from 75% pre-Delta to 53% when Delta became dominant. It didn't differentiate between asymptomatic, symptomatic and severe infections.
- Another used data from 21 hospitals to estimate the mRNA vaccines' effectiveness against hospitalization over time, and found there was no significant change in effectiveness from mid-March to mid-July.
- The third, using New York state data, found that all three vaccines' effectiveness against infection dropped from 92% in early May to 80% at the end of July, but the effectiveness against hospitalization remained relatively stable.
Reality check: This is all good news for most vaccinated people — your vaccines will keep you alive and out of the hospital. - It's not so great for some vulnerable populations, particularly nursing home residents, who may be less protected than they'd thought.
- "Additional evaluations are needed to understand whether protection against severe disease in nursing home residents is also declining over time," the nursing home study warns.
The bottom line: The Biden administration's worst nightmare is finding out about declining effectiveness through a spike in real-world death rates. They've instead decided to get ahead of the virus. Share this story. |
    |
| |
| |
| 2. Biden administration ramps up pressure |
 |
|
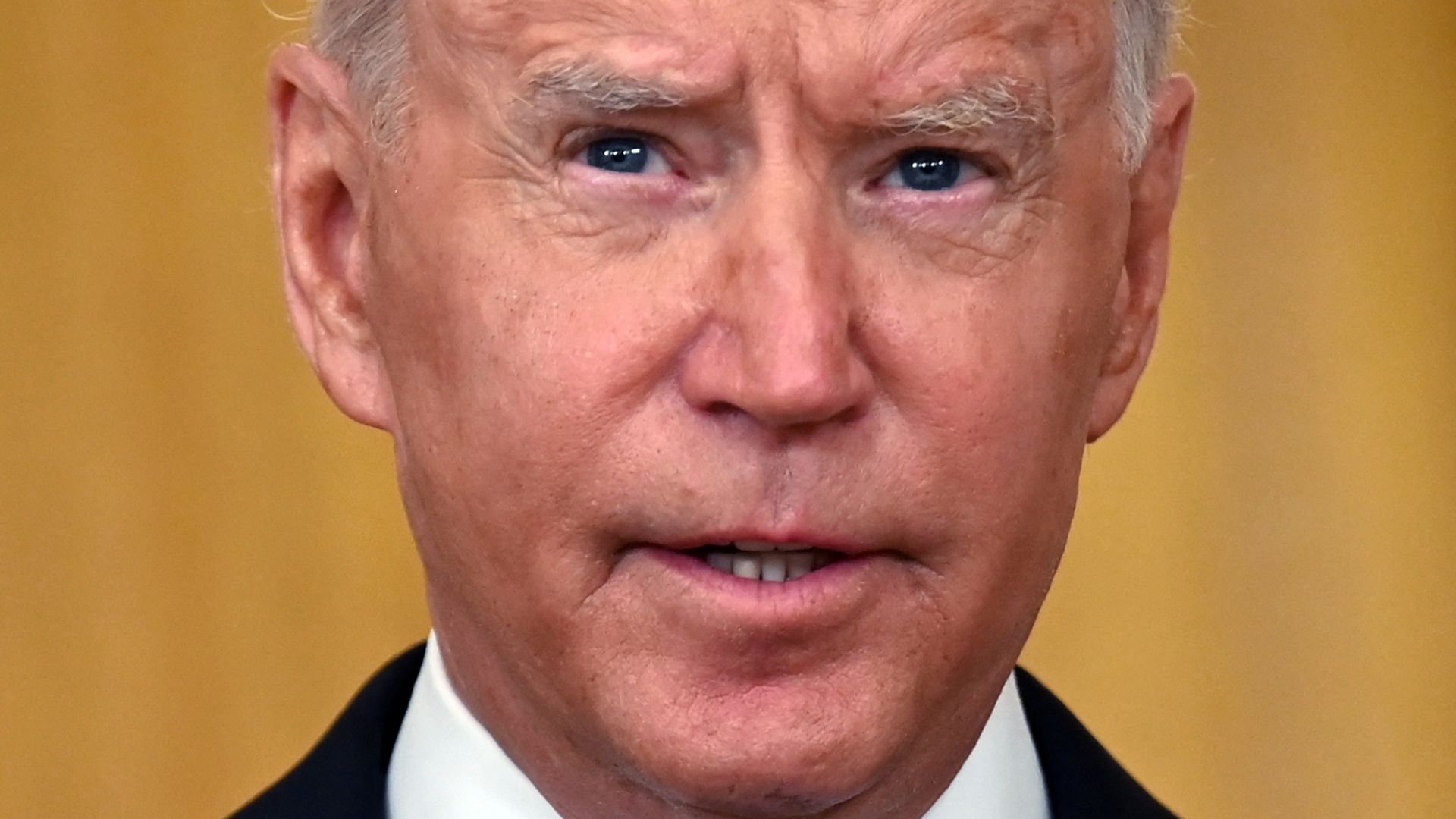
| President Biden. Photo: Jim Watson/AFP via Getty Images |
| |
| President Biden signaled Wednesday he's leaning in when it comes to taking a heavier-handed approach to the administration's COVID response. Driving the news: In addition to backing boosters (see above), Biden unveiled plans to require U.S. nursing home staff be vaccinated, or risk federal funding. He also stepped up his fight with GOP governors over state bans to school mask mandates. "As I've said before, 'If you're not going to fight COVID-19, at least get out of the way of everyone else who is trying," Biden said during a briefing at the White House. - But some critics said the administration may have played too heavy of a hand, increasing pressure on the FDA and CDC with its announcement of boosters for the general public before either had a chance to consider and approve them.
Zoom in: Vaccination rates among nursing home staff — who work with some of the most vulnerable patients — have remained stubbornly low, with about 62% of staff vaccinated as of Aug. 8. The other side: But the industry, which already struggles with a shortage of workers, could "face a disastrous workforce challenge" that could harm the quality of care. - "Focusing only on nursing homes will cause vaccine-hesitant workers to flee to other health care providers and leave many centers without adequate staff to care for residents," warned Mark Parkinson, CEO of the American Health Care Association and National Center for Assisted Living.
Go deeper. |
    |
| |
| |
| 3. America's Delta toll |
 Data: CSSE Johns Hopkins University; Note: Kansas data via CDC and from Aug. 3-16, 2021; Map: Axios Visuals The number of coronavirus cases in most states is still rising, ensuring that the U.S. has a long way to go in its fight against the Delta variant, Caitlin reports. Why it matters: Hospitals across the country are filling up with coronavirus patients, and some are running out of available ICU beds. Between the lines: Cases rose most in the Upper Midwest, Washington state, West Virginia and Washington, D.C. - Some of the states hit hardest by Delta early on, like Missouri, Arkansas and Louisiana, saw a plateau in cases, a hopeful sign that their caseloads could soon start to decline.
- Cases rose by 12.6% in Florida, which continues to set hospitalization records that exceed the levels reached before vaccines were widely available.
What we're watching: The Delta wave will likely burn out eventually, but it's anyone's guess as to when. - On the positive side, the spike in hospitalizations and deaths appears to have prompted a bump in U.S. vaccination rates.
- On the other hand, Americans burned out on social distancing, combined with schools full of unvaccinated children — many of whom aren't required to wear masks — could provide ample fuel for the virus.
|
    |
| |
| |
| A message from the Coalition Against Surprise Medical Billing |
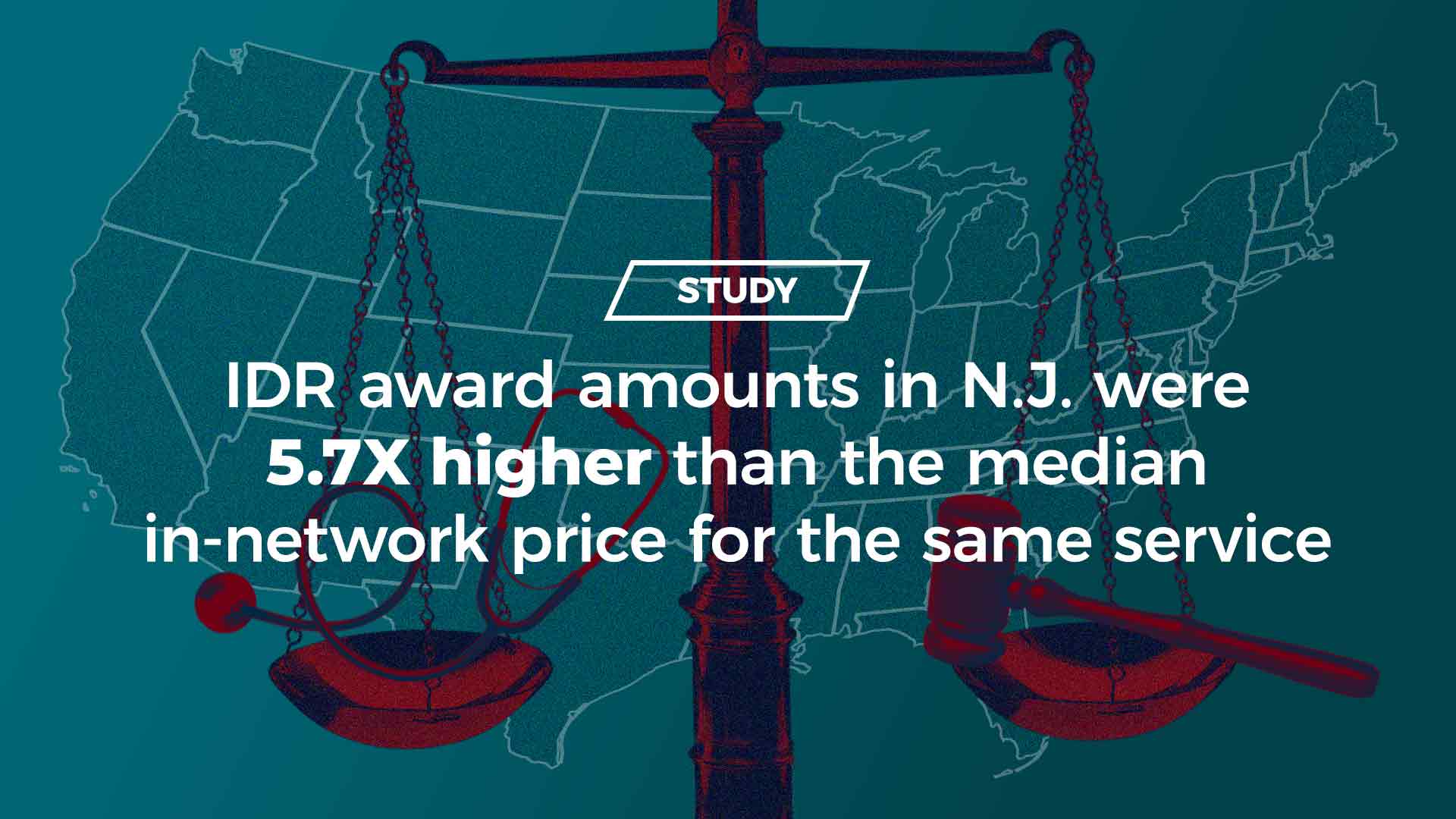
| IDR leads to inflated charges and higher costs for consumers |
| |
 |
| |
| Any Independent Dispute Resolution (IDR) process that relies on providers' inflationary charges for final payment will lead to higher costs for consumers — as shown in New Jersey, New York and Texas. What this means: Federal regulations must limit IDR and protect patients. Learn more. |
| |
| |
| 4. Yep, there's a code for that |
| The American Medical Association has created new billing codes so insurance programs can pay doctors, hospitals and others to administer a third dose of the Pfizer and Moderna COVID-19 vaccines, Axios' Bob Herman writes. Between the lines: America's medical billing systems are ready to go even though the federal policy on widespread booster doses still requires a thumbs-up from the FDA and the CDC's expert vaccine panel. Worth reminding: The vaccines are still free for everyone, which means you don't have to pay anything out of pocket for a shot. - Medicare pays providers $40 for each vaccine dose given.
|
    |
| |
| |
| 5. What about Johnson & Johnson? |
 |
|
| Illustration: Aïda Amer/Axios |
| |
| The 14 million people who received a Johnson & Johnson shot are going to have to wait a few more weeks for answers on boosters due to lack of data, Axios' Marisa Fernandez reports. Why it matters: The CDC currently advises people to stay with the shot they had initially. The effects of mixing doses are still unclear, but "it is anticipated that vaccine boosters will likely be needed," the White House tweeted. - Data for the J&J shot is months behind mRNA shots because the company only received emergency use authorization in March, while Pfizer and Moderna received theirs in December.
Still, emerging evidence shows people who received adenovirus vaccines like J&J or AstraZeneca would benefit from an additional dose of an mRNA vaccine. - Countries like Germany and the UK have been giving doses of mRNA vaccines to people who got the AstraZeneca vaccine, BBC reports.
What we know: Booster recommendations for J&J recipients were largely left out of the conversation last week when federal health officials announced that immunocompromised Americans can receive an additional dose of the COVID-19 vaccine. - J&J anticipates sharing data shortly regarding boosting with its COVID-19 vaccine, a spokesperson tells Axios.
Read more. |
    |
| |
| |
| 6. Catch up quick |
- The EPA will block a pesticide tied to neurological harm in children (New York Times)
- Small businesses are suing New York City over indoor vaccine mandate (Axios)
- Washington state announced the strictest school vaccine mandate in U.S. (Axios)
|
    |
| |
| |
| A message from the Coalition Against Surprise Medical Billing |
| Surprise medical billing regulations must protect patients |
| |
 |
| |
| Congress ended surprise billing, but the fight is not over yet. It's up to the Administration to protect patients from higher health care costs. To do this, regulators must limit the Independent Dispute Resolution (IDR) process and prevent private equity from gaming the system. Learn more. |
| |
 | | It'll help you deliver employee communications more effectively. | | |







No comments:
Post a Comment