| |
| |
| |
| Presented By PhRMA |
| |
| Axios Vitals |
| By Tina Reed · Nov 01, 2022 |
| 🦃 Happy First Day of November, Vitals readers. Can you believe there are only 60 days left in 2022? Today's newsletter is 997 words or a 4-minute read. |
| |
| |
| 1 big thing: The search for an RSV vaccine |
 |
|
| Illustration: Brendan Lynch/Axios |
| |
| Fears of a winter "tripledemic" have brought warnings to get flu shots and reformulated COVID boosters. But there are no such options for the third pathogen in circulation: respiratory syncytial virus, or RSV. Driving the news: This morning, Pfizer announced promising topline results of a late-stage clinical trial for an experimental RSV vaccine. The vaccine would offer protection to infants from birth by vaccinating women while they're still pregnant. - The vaccine showed 82% efficacy against severe illness through the first 90 days of life and 69% through the first six months of life, the company said in a statement.
- Pfizer officials said they intend to submit for Food and Drug Administration approval by the end of the year.
State of play: This is one of several RSV candidates nearing FDA review, per Nature. - White House COVID-19 adviser Ashish Jha told CNN he's "hopeful" there could be an RSV vaccine available by next fall.
Why it matters: We're experiencing a particularly virulent season when it comes to RSV. - The virus has symptoms similar to the common cold but can be life-threatening for infants, young children and the elderly. It's already stretched some pediatric hospitals to capacity.
- The virus is circulating while influenza is off to an early start and new, troubling COVID variants are emerging.
Yes, but: Most of the other RSV candidates are aimed at older adults. The bottom line: All of the work won't yield an RSV shot this season, but there are options on the horizon, officials say. - In the meantime, U.S. officials are urging caution for vulnerable populations, including using the COVID and flu tools we do have.
Go deeper. |
    |
| |
| |
| 2. Millions of ACA signups may duck premium hikes |
 |
|
| Illustration: Lindsey Bailey/Axios |
| |
| Open enrollment for Affordable Care Act coverage begins today, with enhanced subsidies that Congress renewed through 2025 expected to cushion the blow of premium increases for millions of Americans, Axios' Arielle Dreher writes. The big picture: Health costs are steadily climbing due to inflation and a post-pandemic surge in demand for medical services. - But the more than 12 million Americans now receiving subsidies will likely benefit from them again in 2023, including those making more than 400% of the federal poverty level.
- The amount people pay in premiums will also be limited to 8.5% of their income.
- And the Biden administration finalized rules to fix a glitch that had been preventing some families from getting subsidized health insurance.
Yes, but: For those who don't qualify for subsidies, premiums will increase more than in past years for marketplace plans. Related: Shopping for ACA health insurance? Here's what's new (NPR) |
    |
| |
| |
| 3. CMS offers reprieve on home health payments |
 |
|
| Illustration: Sarah Grillo/Axios |
| |
| Home health providers will avoid significant Medicare pay cuts next year, after the Biden administration on Monday announced a net 0.7% increase in fees, Axios' Maya Goldman writes. - But the industry is still pushing Congress to delay future rate cuts.
Why it matters: The $125 million increase is a reprieve of sorts after the Centers for Medicare and Medicaid Services proposed an $810 million cut in June. Providers hinted at legal action following the proposal. - Instead, reductions will be phased in over two years, spreading out the pain for a health sector that's grappled with staffing shortages and rising costs.
Look ahead: Sens. Susan Collins (R-Maine) and Debbie Stabenow (D-Mich.) have introduced a bill to push off the cuts until 2026. But the legislation may not get taken up before the end of the year, and the bill doesn't get at the agency's root cause for the cuts. - Additionally, CMS still plans to claw back the extra $2 billion it paid to home health providers in 2020 and 2021 as a result of the new payment system. A roadmap for that could come in next year's rule.
Read the rest. |
    |
| |
| |
| A message from PhRMA |
| How insured Americans navigate unclear insurance coverage |
| |
 |
| |
| According to new findings, insured Americans favor policy solutions that improve their ability to navigate and access their care while lowering their out-of-pocket costs. An example: Tackling the barriers introduced by insurers and middlemen like pharmacy benefit managers. Read more. |
| |
| |
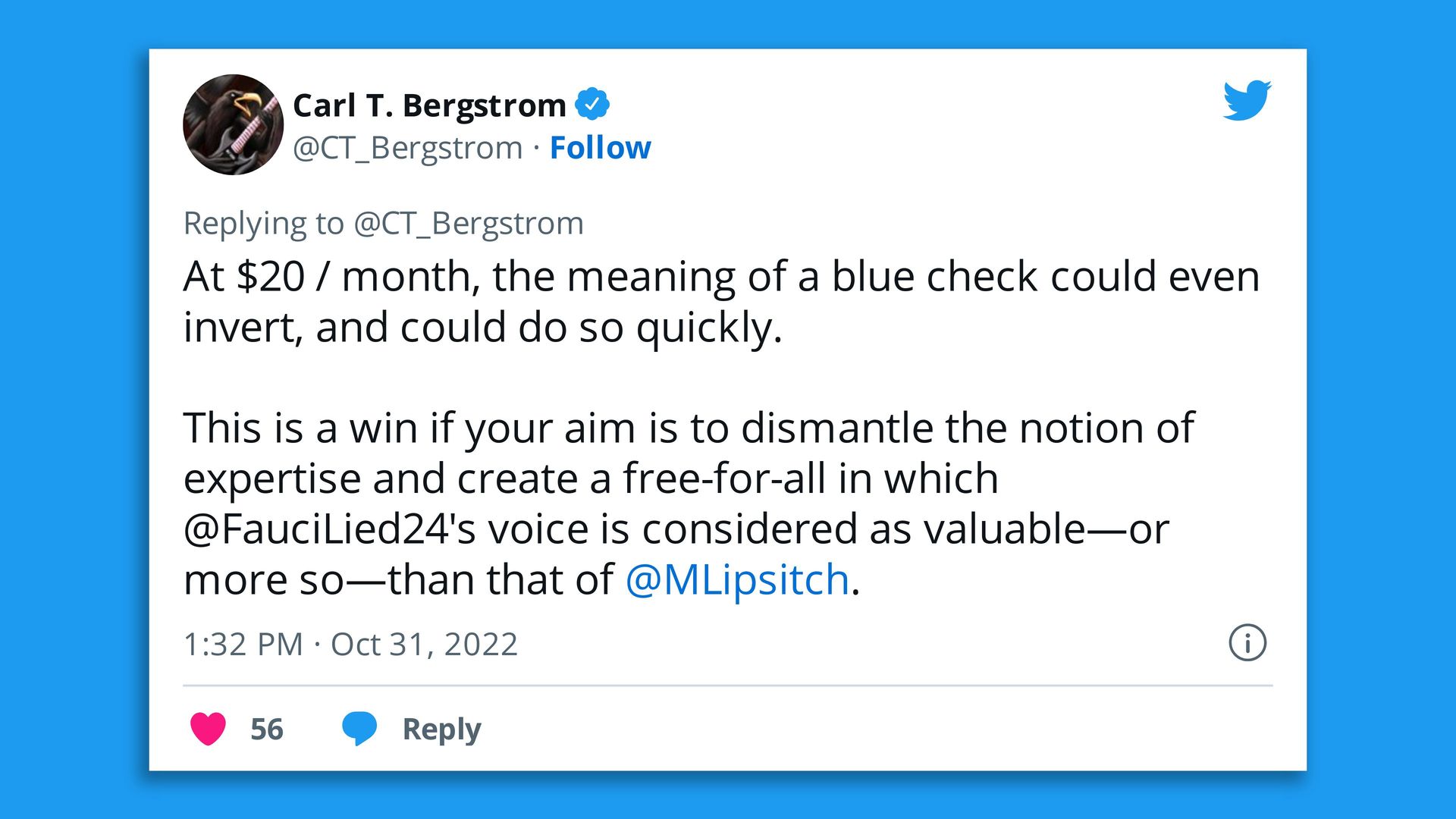
| 4. Quote du jour: Health care's Twitter problem |
 |
|
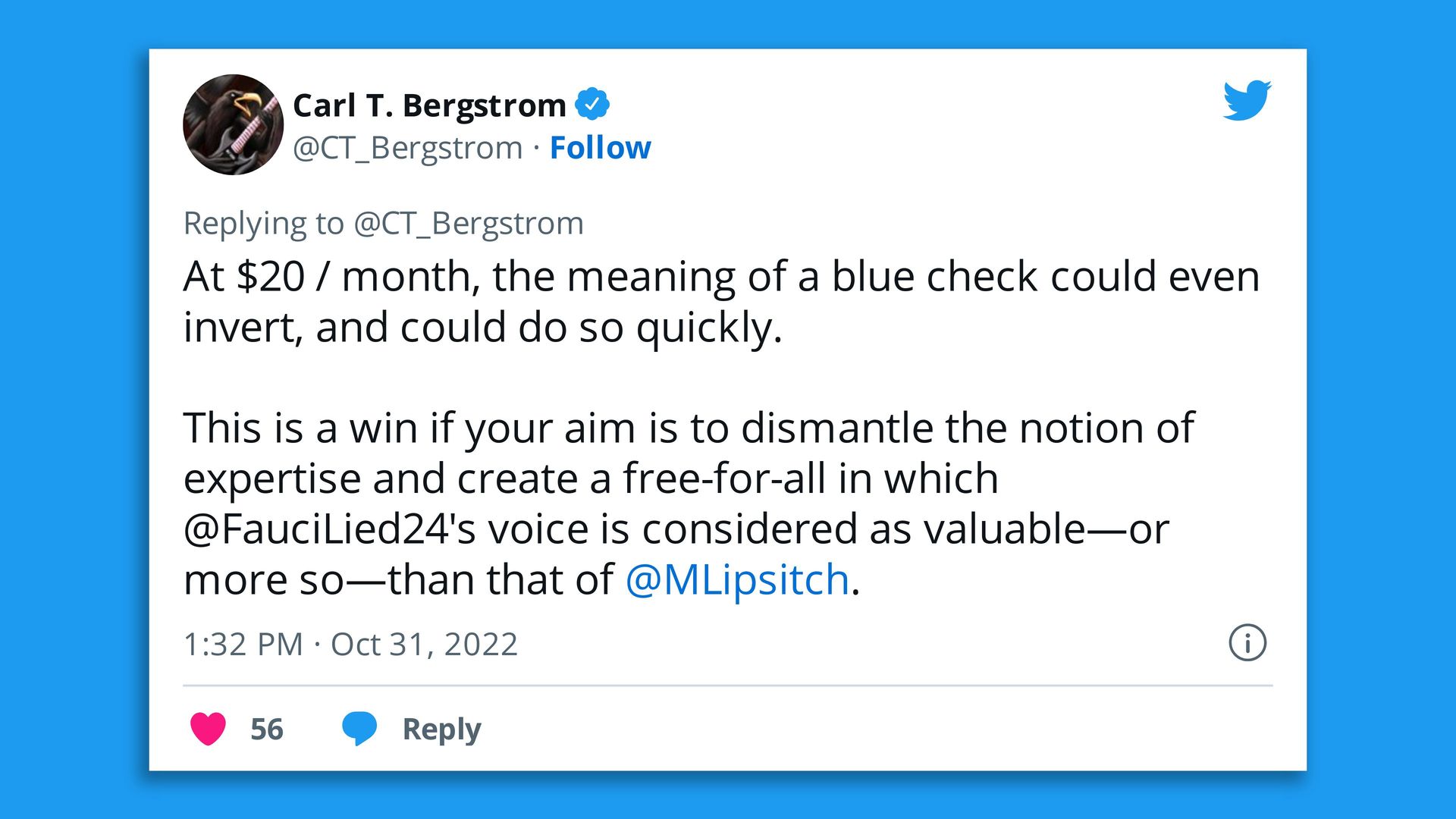
| Screenshot: @CT_Bergstrom/Twitter |
| |
| Under Elon Musk's ownership, Twitter may charge up to $20 a month to get or keep the blue check mark that verifies a user's identity. Why it matters: While it's far from perfect, the blue check proved important for identifying legitimate sources on the pandemic during what was at times a swirl of misinformation. What to watch: If the surcharge is imposed and enough doctors and health authorities balk, it could become hard to parse valuable health information from the platform in the future. |
    |
| |
| |
| 5. Study shows anesthesia use disparities |
 |
|
| Photo illustration: Brendan Lynch/Axios. Photo: Linh Ta |
| |
| New research showing racial disparities in regional anesthesia use has major implications for Black women — especially in pregnancy and childbirth, experts tell Axios' Shawna Chen. Why it matters: Black women have a long history of experiencing medical maltreatment, the legacy of which remains today in implicit biases and systemic inequities that worsen health outcomes. Driving the news: A new study, which reviewed the records of nearly 57,000 adults who had surgery between 2016 and 2021, found that people of color were 29% less likely to receive regional anesthesia compared to white patients. - Patients with Medicaid insurance were 39% less likely to receive regional anesthesia than those with private insurance.
The big picture: That Black women are less able to access anesthesia has particularly dangerous consequences in pregnancy and childbirth. - Black women have a 53% increased risk of dying in the hospital during childbirth compared to white women — no matter their income level, type of insurance or other social determinants of health, according to another recent survey.
- Researchers have also shown that the use of epidurals in childbirth is associated with a decreased risk of severe maternal morbidity.
|
    |
| |
| |
| 6. Catch up quick |
| 🩺 California patients who rely on dialysis worry about the fallout from a third ballot measure attempt to more tightly regulate the industry. (KHN) ✈️ The Supreme Court let stand a ruling that allows the TSA to require mask-wearing on planes, trains and other forms of transportation. (The Hill) 👀 The FDA says providers offering medication abortion before pregnancy have gone rogue. (Politico) 💉 There is a record number of outbreaks of cholera around the world and the vaccine supply is being strained enough that health officials are rationing supplies. (New York Times) |
    |
| |
| |
| A message from PhRMA |
| Americans want policy reforms that improve their insurance |
| |
 |
| |
| Did you know 39% of insured Americans say they don't understand what's covered by their insurance? Health insurance coverage should be predictable and transparent, and insured Americans agree. Learn more from PhRMA's latest Patient Experience Survey report. |
| |
| Thanks for reading, and thanks to senior editor Adriel Bettelheim and senior copy editor Bryan McBournie for the edits. Please ask your friends and colleagues to sign up. |
 | | Why stop here? Let's go Pro. | | |







No comments:
Post a Comment