| |
| |
| |
| Presented By the Coalition Against Surprise Medical Billing |
| |
| Axios Vitals |
| By Tina Reed ·Aug 18, 2021 |
| Hello Vitals readers. Today's newsletter is 875 words, or a 3-minute read. Situational awareness: The White House coronavirus team will today address the subject of boosters in a briefing, and the president will speak after, White House press secretary Jen Psaki said yesterday. |
| |
| |
| 1 big thing: The case for boosters |
 |
|
| Illustration: Annelise Capossela/Axios |
| |
| The Biden administration's decision to offer COVID boosters to most Americans is an effort to stay ahead of declining vaccine effectiveness, Axios' Caitlin Owens writes. Why it matters: Even with more than half the population fully vaccinated — well above most of the rest of the world — the coronavirus is still causing a domestic crisis. And it could get worse if efficacy against severe illness also starts to wane. - "No one wants to have decreasing vaccine efficacy against severe disease when you're seeing it decrease against mild to moderate disease. You want to get ahead of that," a senior Biden official told Axios.
Driving the news: The administration is eyeing a plan to give boosters around eight months after the first round of vaccines. - New CDC data showing a drop in vaccine effectiveness over time — viewed by the administration's COVID task force over the weekend — ultimately prompted the decision, Politico reported yesterday.
The big picture: Data released by other countries and non-governmental researchers has shown a significant decline in the vaccines' effectiveness against infection. - However, no data has yet shown a big decline in their effectiveness against severe disease.
- It's unclear whether the decline is because the vaccines are waning, or the strength of the Delta variant, or both. Breakthrough cases are more dangerous for some populations, like the elderly, than others.
What they're saying: "Effectiveness against severe disease may have held, but you don't know how long it'll hold," said a source close to the administration. "If you know effectiveness declines and you know you can increase your immunity, why wouldn't you?" - "You are conservative in your planning or else you risk a lot of bad outcomes in vulnerable people," the source added.
G0 deeper. |
    |
| |
| |
| 2. The case against boosters |
 |
|
| Illustration: Rae Cook/Axios |
| |
| The idea of approving COVID-19 boosters for the general population fails fundamental ethics tests, Axios' Bob Herman writes. Why it matters: There's still a global shortage of vaccines. Physicians and medical ethicists say it's difficult to justify a third dose for relatively healthy people in the U.S. when many others haven't gotten their first. The big picture: An approved third dose for the immunocompromised is reasonable, ethicists say, because three doses should have been their default regimen, and it will give a boost in protection to a group that is more likely to end up in the hospital from COVID-19. Yes, but: "Once you get to anybody who wants to get a third dose, then I think other people in other countries start to have a rightful basis for complaint," said Govind Persad, a health policy and ethics professor at the University of Denver. The bottom line: "The Delta variant didn't come from nowhere," Faden said. "To have a better chance of containing this pandemic, we have a self-interested reason in seeing vaccination coverage go up in people outside of our country." Share this story. |
    |
| |
| |
| 3. Disparities in health spending |
 Data: Dieleman, et al., 2021, "U.S. Health Care Spending by Race and Ethnicity, 2002-2016;" Chart: Axios Visuals Per-person health spending is highest for white individuals compared to patients of other races, even after adjusting for factors like age and health conditions, according to a study led by the Institute for Health Metrics and Evaluation in Seattle. By the numbers: Of the $2.4 trillion spent across six types of care included in this study, per-person spending for white individuals averaged $8,141 and accounted for 72% of health care spending. - Per-person spending was the lowest, at an average of $4,692, for Asian, Native Hawaiian, and Pacific Islander individuals.
- The average per-person spending for Black individuals and Hispanic individuals was $7,361 and $6,025, respectively.
Read more. |
    |
| |
| |
| A message from the Coalition Against Surprise Medical Billing |
| Surprise medical billing regulations must protect patients |
| |
 |
| |
| Congress ended surprise billing, but the fight is not over yet. It's up to the Administration to protect patients from higher health care costs. To do this, regulators must limit the Independent Dispute Resolution (IDR) process and prevent private equity from gaming the system. Learn more. |
| |
| |
| 4. Quote du jour: Angling for a deal |
| "We need a release that's sufficient to get our goals accomplished ... If the release fails to do that, we will not support it." — David Sackler, part of the family that owns OxyContin maker Purdue Pharma, at a Tuesday court appearance. He said the family won't contribute billions of dollars to a legal settlement unless they're freed from all current and future lawsuits over the company's activities, the Associated Press reported. |
    |
| |
| |
| 5. Heatwaves' hit to hospitals |
 |
|
| Portland residents stay cool in a public fountain filled with soap suds during a heatwave. Photo: Nathan Howard/Getty Images |
| |
| The extreme heatwaves that stagnated over the Pacific Northwest this summer exposed a new reality for hospitals overwhelmed by patients with heat-related illnesses, Axios' Marisa Fernandez reports. Why it matters: State and local health departments in Washington and Oregon report those who succumbed to heat-related illness were often older, with pre-existing conditions and had no air conditioning. - Officials say they expect this summer's heat is only a preview of what to expect in the future.
What's happening: Heat-related hospitalizations typically peak in Oregon at 81°F, according to a 2019 study. - The state reached 116°F in late June, which contributed to a staggering 1,038 visits to the ER in Washington and Oregon that occurred on June 28 alone, the CDC said.
- "When you aren't used to extreme heat, you may not actually realize how dangerous it is," said Renee Salas, emergency medicine physician at Massachusetts General Hospital, during an event hosted by the Harvard T.H. Chan School of Public Health on Tuesday.
The bottom line: Long term, they say, major infrastructure overhauls and better electronic medical reporting will need to monitor heatwaves and better respond. |
    |
| |
| |
| 6. Catch up quick |
- Federal vaccine program hasn't helped those whose lives were altered by COVID shot. (KHN)
- Delayed Wuhan report adds crucial detail to COVID origin puzzle. (Bloomberg Businessweek)
- In COVID-19 vaccination push, Latin American nations are catching up to the U.S. (WSJ)
|
    |
| |
| |
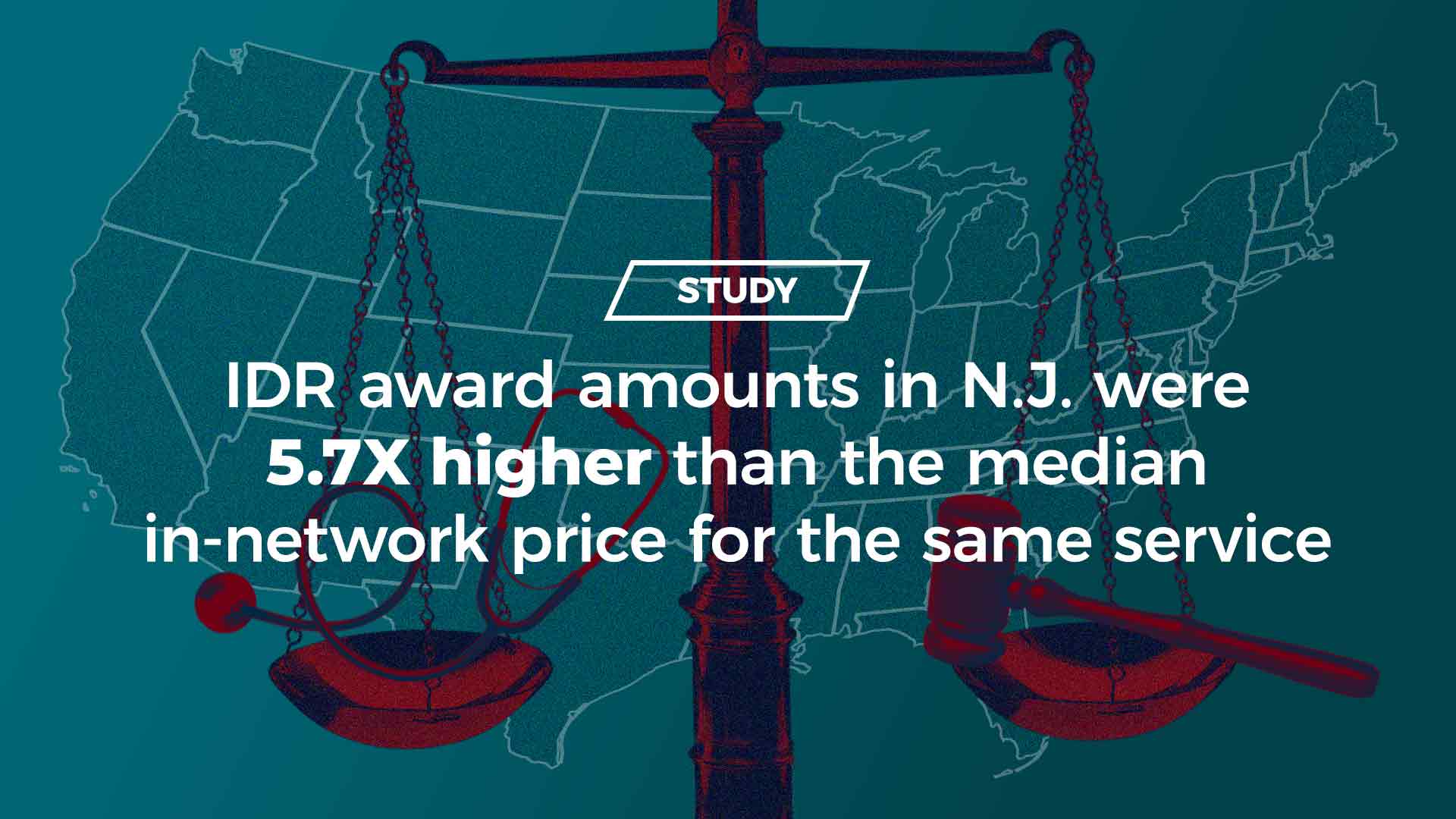
| A message from the Coalition Against Surprise Medical Billing |
| IDR leads to inflated charges and higher costs for consumers |
| |
 |
| |
| Any Independent Dispute Resolution (IDR) process that relies on providers' inflationary charges for final payment will lead to higher costs for consumers — as shown in New Jersey, New York and Texas. What this means: Federal regulations must limit IDR and protect patients. Learn more. |
| |
 | | It'll help you deliver employee communications more effectively. | | |







No comments:
Post a Comment