| |
| |
| |
| Presented By the Coalition Against Surprise Medical Billing |
| |
| Axios Vitals |
| By Tina Reed ·Aug 20, 2021 |
| 😎 The weekend is almost here, Vitals readers. But first, today's newsletter is 1,036 words or a 4-minute read. |
| |
| |
| 1 big thing: The importance of vaccine timing |
 |
|
| Illustration: Sarah Grillo/Axios |
| |
| The amount of time between COVID vaccine doses may have an impact on the durability of the protection the vaccine offered, experts say. Why it matters: The three- or four-week interval between the first- and second-doses of the mRNA vaccines produced by Pfizer-BioNTech and Moderna was relatively short by vaccine standards — and explains why U.S. officials' interest in boosters due to waning immunity isn't entirely surprising. To be clear, the CDC recommends individuals who get one of the mRNA shots to get their second shot as close to the recommended three-week or four-week interval after their first shot as possible. - But there's a broader discussion happening among some infectious disease experts about the impact of vaccine dose timing.
- "When you make that decision to do a three- or four-week interval, it sacrifices length of protection and durability of protection," said Peter Hotez, dean of the National School of Tropical Medicine at Baylor College of Medicine in Houston.
- He said it was a smart decision to pursue that vaccine timeline early on "because so many Americans were losing their lives from COVID — 3,000 deaths per day — and we had to get people fully immunized," he said. But it also made boosters much more likely, he said.
- Longer intervals between doses in a multi-dose vaccine regimen may allow the immune system time to mature, or allow antibodies to improve in quality while dwindling in number, John Moore, a professor of microbiology and immunology at Weill Cornell Medicine in New York told MedPage Today.
The bottom line: At the very least, experts say the eight-month gap in the interval that the U.S. may follow for third doses could offer a long-lasting boost. - "That may be it for a while, we may not need annual boosters," Hotez told MedPage. "This could be the third and done."
Share this story. |
    |
| |
| |
| 2. Hospitalizations are getting more expensive |
| Coronavirus patients who end up hospitalized — the vast majority of whom are unvaccinated — are increasingly likely to be on the hook for their medical bills, Axios' Caitlin Owens reports from a new KFF analysis. Where it stands: Early in the pandemic, most insurers waived out-of-pocket costs for coronavirus hospitalizations. - But with vaccines readily available, many patients are once again on the hook for deductibles and co-pays, which could make remaining unvaccinated a lot more expensive.
By the numbers: KFF surveyed the two largest insurers in each state and the District of Columbia, and found that 72% of them had stopped waiving cost-sharing requirements for coronavirus treatment as of this month. - In the first half of the year, about a third of employers offering health benefits said their largest available plan waived cost-sharing obligations for COVID treatment.
Between the lines: The typical deductible in an employer health plan is $1,644, per KFF, and hospitalization for coronavirus treatment could amount to around $1,300 in out-of-pocket costs. What we're watching: Vaccinated people rarely need to be hospitalized, even if they contract the virus, at least according to data that's been published so far. - Even if that changes, part of the reason insurers initially waived out-of-pocket treatment costs was because they were paying out less than they expected to in medical claims.
- Unless people once again stop seeking care like they did in spring 2020, it seems unlikely that insurers will reverse course.
|
    |
| |
| |
| 3. The case for getting kids back to school |
 Reproduced from KFF; Chart: Axios Visuals Parents are much more likely to report their kids are experiencing negative effects if they are going to school virtually during the pandemic than if they attend school in person, writes Drew Altman, KFF's president and CEO. Why it matters: The findings from the KFF Vaccine Monitor underscore the importance of keeping kids in school in person — which means doing it safely, with masking. By the numbers: 47% of parents whose kids attended school virtually or in a hybrid model during the last school year say they fell behind academically compared with 26% of parents whose kids attended all or mostly in person. - 46% of parents say their kids attending schools virtually fell behind in their social and emotional development, compared with 31% of parents whose kids attended school in person.
- 22% of parents whose kids who went to school say their kids experienced mental health or behavioral problems due to COVID, but the number rose to 39% for kids whose school experience was largely through a computer screen.
The bottom line: The findings reinforce the urgency of getting students and school personnel vaccinated as soon as possible. Read more. |
    |
| |
| |
| A message from the Coalition Against Surprise Medical Billing |
| Surprise medical billing regulations must protect patients |
| |
 |
| |
| Congress ended surprise billing, but the fight is not over yet. It's up to the Administration to protect patients from higher health care costs. To do this, regulators must limit the Independent Dispute Resolution (IDR) process and prevent private equity from gaming the system. Learn more. |
| |
| |
| 4. Extreme heat is a global health crisis |
 |
|
| Illustration: Sarah Grillo/Axios |
| |
| More than 356,000 people died from causes related to extreme heat in just nine countries in 2019, Axios Marisa Fernandez reports from a pair of studies published Thursday in The Lancet. What's next: The death toll is expected to grow as temperatures increase worldwide, the authors say. By the numbers: One of the studies analyzed about 65 million deaths in nine countries — encompassing 95% of the inhabited global temperature range and 29% of the global population. - Heat-related deaths increased by 74% between 1980 and 2016.
- About 1.3 million people died from extreme cold during the same time period.
Go deeper. |
    |
| |
| |
| 5. Business notes |
- David Feinberg is ditching Google's health venture to be CEO of electronic health record giant Cerner. (Also noteworthy: Cerner has a 10-year deal with Geisinger, which Feinberg led before Google.)
- Johnson & Johnson CEO Alex Gorsky is stepping aside, the Wall Street Journal reported. He'll be replaced by Joaquin Duato, who led J&J's pharmaceuticals business before becoming a Gorsky deputy.
- Inovalon, a data analytics company used by almost every major health care company, agreed to go private in a $7.3 billion deal led by private equity firm Nordic Capital.
- AbbVie and J&J won a court fight involving their cancer drug Imbruvica. A judge said a competing generic drug infringed on Imbruvica's patents, ensuring no generic entry until 2032.
|
    |
| |
| |
| 6. Dog of the week |
 |
|
| Hannah. Photo: Joe Reblando. |
| |
| Meet Hannah, a six-year old Boston terrier who was adopted from the Old Dominion Boston Terrier Rescue. - Hannah lives in Vienna, Virginia, with dad Joe Reblando, founder of Reblando Public Relations. But she's often out and about on the D.C., Virginia, and Atlanta bar scenes in her travel bag. (She's even 0n Insta.)
- "Like most Bostons, Hannah farts up a storm and snores like an old man, but I think that's part of her charm!" Reblando said.
|
    |
| |
| |
| A message from the Coalition Against Surprise Medical Billing |
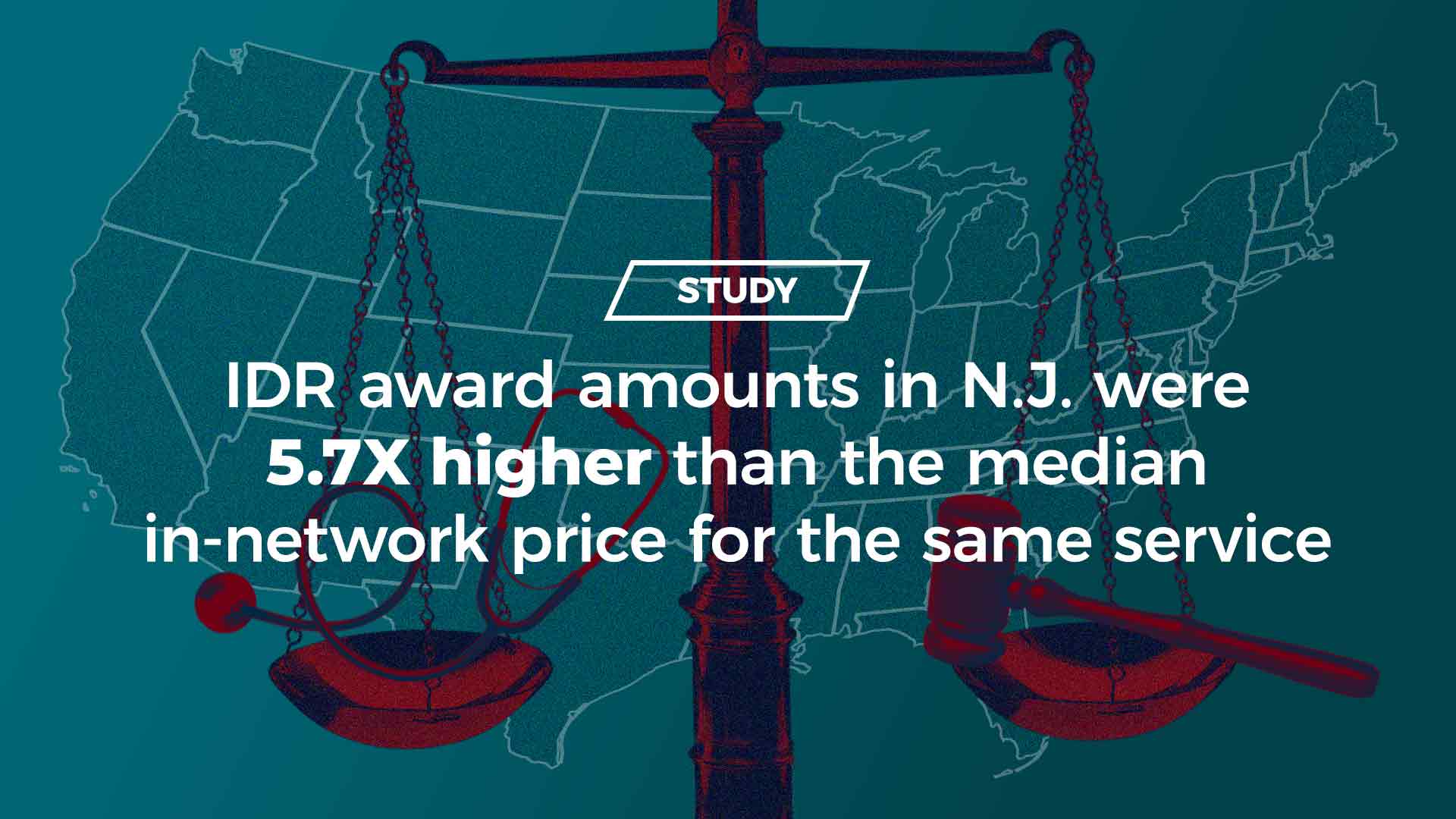
| IDR leads to inflated charges and higher costs for consumers |
| |
 |
| |
| Any Independent Dispute Resolution (IDR) process that relies on providers' inflationary charges for final payment will lead to higher costs for consumers — as shown in New Jersey, New York and Texas. What this means: Federal regulations must limit IDR and protect patients. Learn more. |
| |
| 👍 Thanks for reading! Got this email from a co-worker, family member or friend? Sign up here. |
 | | It'll help you deliver employee communications more effectively. | | |







No comments:
Post a Comment