| |
| |
| |
| Presented By UnitedHealth Group |
| |
| Axios Vitals |
| By Tina Reed · Sep 13, 2022 |
| Happy Tuesday, Vitals readers. Today's newsletter is 1,022 words or a 4-minute read. |
| |
| |
| 1 big thing: Why we need to be talking about vaccines that offer "mucosal immunity" |
 |
|
| Illustration: Shoshana Gordon/Axios |
| |
| As the U.S. rolls out updated mRNA-based COVID shots, a growing chorus of experts say it's a mistake not to focus on treatments that boost immunity through mucous membranes. Why it matters: Next-generation oral or nasal vaccines could quickly boost the immune response in the very airways where COVID-19 enters the body and ultimately break our reliance on reformulated shots to target the latest variants of concern. - But the U.S. isn't putting money into such products.
Driving the news: China made headlines this month for the emergency approval of CanSino's inhaled COVID-19 vaccine. Last week, India approved Bharat Biotech's intranasal vaccine for emergency use. - Both claim to stimulate mucosal immunity, which not only protects against the virus, but blocks it from spreading.
- They come on the heels of research in Science Immunology this summer saying mucosal booster vaccination is needed to establish robust "sterilizing immunity" against COVID.
State of play: Experts say mRNA shots did a remarkable job protecting against infection and the spread of earlier strains of COVID. They also continue to keep people from being hospitalized or dying. - But they don't prevent transmission in a way that could actually end the pandemic.
- Eric Topol, executive vice president of Scripps Research, points to the number of reinfections as the more contagious Omicron variant swept the nation.
- "That signified that we had a leak. A big leak. That leak is the fact Omicron has become so much more transmissible, so much more able to get into our upper airway," Topol said.
- The answer he, and other experts say, could lie in vaccines that work in the membranes where respiratory diseases take root.
Be smart: Mucosal membranes are the moist, inner lining of some organs and body cavities, such as the nose, mouth, lungs, and stomach. - Mucosal immunity is a key compartment in our immune system, different from the antibody response in the blood that's stimulated by vaccine shots, said Michael Mina, an epidemiologist and chief scientific officer for at-home testing company eMed.
Go deeper. |
    |
| |
| |
| 2. Axios-Ipsos poll: Roll credits on the pandemic |
 Data: Axios/Ipsos poll; Chart:Simran Parwani/Axios Two and a half years into the pandemic, Americans say they're doing well in most aspects of their lives — except possibly their personal finances, Axios' Adriel Bettelheim writes about the latest installment of the Axios/Ipsos Coronavirus Index. Why it matters: Many appear ready to roll the credits on the pandemic, despite lingering political divisions over the response and residual distrust of government and some health institutions. Between the lines: While there haven't been significant behavioral shifts since last spring, there's been an across-the-board improvement in the public's mood. - Overwhelming majorities say they had very or somewhat good physical health (83%), mental health (85%), emotional well-being (84%) and home life (90%).
- But only 78% reported having very or somewhat good personal finances.
What they're saying: "Most Americans have turned the page on the COVID pandemic, even as most acknowledge the virus is likely to be with us for the long term," said Cliff Young, president of Ipsos U.S. Public Affairs. Share this story. |
    |
| |
| |
| 3. Report: Sky-high markups on 340B cancer drugs |
 |
|
| Illustration: Lazaro Gamio/Axios |
| |
| Safety net hospitals are marking up the cost of drugs they buy through the government's discount drug program by as much as 11 times the cost, according to a new report provided first to Axios by the Community Oncology Alliance (COA). Why it matters: It's the latest evidence of how providers can benefit from the federal 340B drug pricing program, which provides discounted medicines to ensure access to low-income patients. - Those markups ultimately drive up the cost of care for cancer patients by thousands of dollars — particularly those with high-deductible health plans or who are paying cash, per the group, which gets funding from the pharmaceutical industry.
What they're saying: "This program has turned into literally an unbelievable cash cow," said Ted Okon, executive director of the COA. Zoom in: The COA examined self-reported drug pricing data for 49 of the top acute care hospitals in 340B that see a disproportionate share of poor patients. - Based on the assumption of they were receiving a 34.7% discount on the average sales price of the drugs, the median markup of the oncology drugs studied was 4.9 times hospitals' acquisition costs.
- The lowest average markup was for the leukemia drug Kymriah (3.2 times). The highest was Faslodex, for breast cancer (11.3 times).
Read the rest. |
    |
| |
| |
| A message from UnitedHealth Group |
| Helping drive affordability and combat high drug costs |
| |
 |
| |
| Beginning in 2023, eligible UnitedHealthcare members will pay $0 out of pocket on five critical medications, including insulin and epinephrine. Learn how we're working to make prescription drugs more affordable for the patients who rely on them most. |
| |
| |
| 4. FDA to consider OTC birth control pills |
 |
|
| Illustration: Gabriella Turrisi/Axios |
| |
| The FDA's decision to consider the first birth control pill that could be sold without a prescription may solve some contraception access problems. But gaps in insurance coverage rules could make it unaffordable for some, Axios' Oriana Gonzalez and Caitlin Owens write. Why it matters: Birth control has been crucial in reducing unwanted pregnancies, and advocates say that making it as widely and easily available as possible is even more important now that abortions are banned in many states. The big picture: "It does broaden the availability of contraception. But there is no single magic bullet to solving all problems with access and affordability issues," said Alina Salganicoff, senior vice president and director of women's health policy for the Kaiser Family Foundation. Driving the news: The FDA on Monday scheduled a joint advisory committee meeting to review HRA Pharma's application for what could be the first over-the-counter birth control pill in the U.S. Between the lines: Eliminating the need for a prescription could make it easier for women to get the pills, especially in areas with a dearth of providers or for people who can't take off work for doctor visits. - But that convenience could mean little if patients have to pay out-of-pocket for their birth control and can't afford it, experts say.
|
    |
| |
| |
| 5. Catch up quick |
 |
|
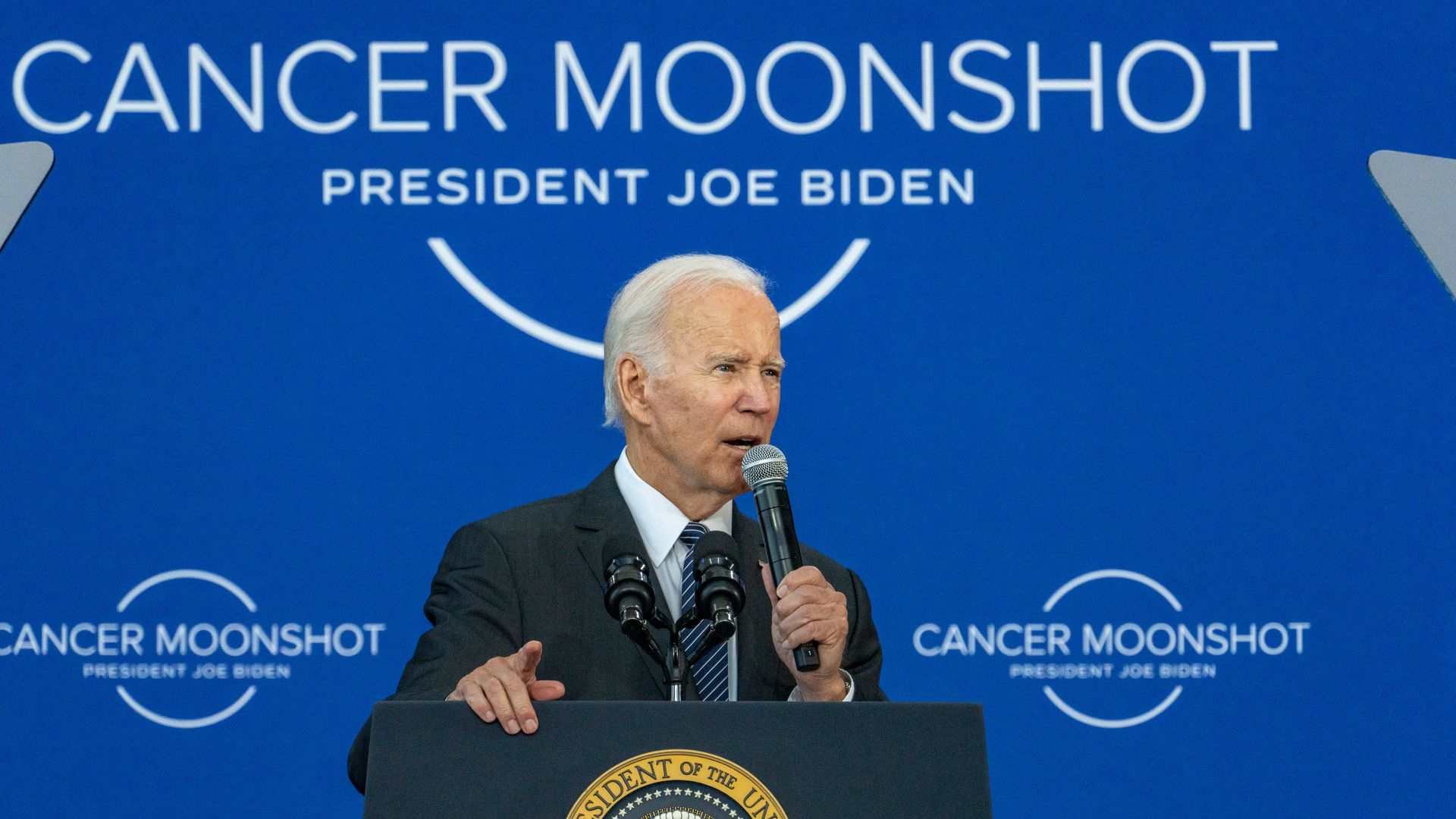
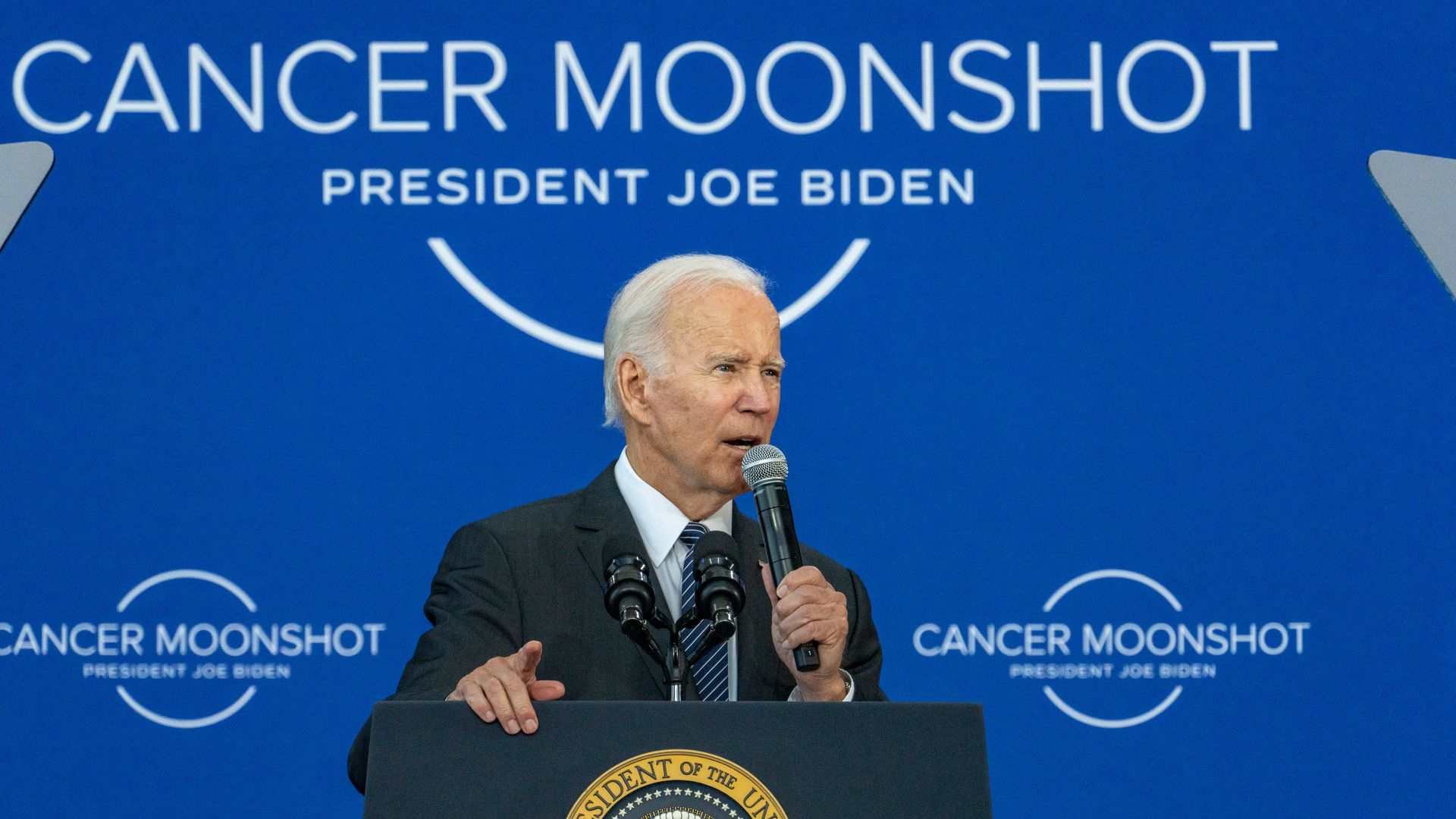
| President Biden speaks at the John F. Kennedy Library and Museum in Boston on Monday. Photo: Vanessa Leroy/Bloomberg via Getty Images |
| |
| 🌙 President Biden took to the road Monday to tout his cancer moonshot, including the signing of an executive order aimed at boosting the domestic biotech industry. (Washington Post) 💉 High-income countries have snapped up monkeypox vaccines and therapeutics, leaving low-income countries, many which have battled the disease for years, with a dearth of options. (New York Times) 🩸 The heel-stick test in newborn babies is considered a crucial public health measure, but the storage of those blood samples — and use for research or even in police investigations years down the road — is gaining new scrutiny. (KHN) |
    |
| |
| |
| A message from UnitedHealth Group |
| Helping lower out-of-pocket costs for consumers |
| |
 |
| |
| Starting in 2023, eligible UnitedHealthcare members will pay $0 out of pocket on critical medications: - Insulin for diabetes.
- Epinephrine for allergic reactions.
- Glucagon for hypoglycemia.
- Naloxone for opioid overdoses.
- Albuterol for acute asthma attacks.
Learn more. |
| |
| 👏 Thanks to Adriel Bettelheim for editing and Bryan McBournie for copy editing today's newsletter. |
 | | Why stop here? Let's go Pro. | | |









No comments:
Post a Comment